- Main Page
- A1C Test
- Advance Directives
- Anxiety
- Aortic Aneurysm
- Aphrodisiacs
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation - AFib
- Back Pain
- Blood Tests
- Blood Test Tubes
- Blood Types
- BMI Calculator
- Body Mass Index - BMI
- Bone Density Scan
- Bone Scan
- BPPV
- Bronchitis
- Cancer - Lung
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- Caregiver Glossary
- Caregiver Resources - LGBTQ+
- Caregiver Resources - MO
- Caregiver Resources - USA
- Continuous Glucose Monitors
- Cholesterol
- Citalopram
- COPD
- Coronary Artery Disease
- Cough
- CPAP
- CT scan
- Cyclobenzaprine
- Degenerative Disc Disease
- Depression
- Diabetes Information
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes Facts
- Diabetes Care
- Diabetes Care Team
- Diabetes & Fruits
- Diabetes - Gestational
- Diabetes - Pre
- Diabetic Terms
- Diabetes & Vegetables
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Disability Permits
- Do Not Resuscitate
- Dupixent®
- Echocardiogram
- E-Cigarettes
- Electrocardiogram
- Electromyography
- Emphysema
- Epidural - Lumbar
- Epidural - Transforaminal
- Epsom Salt
- Facet Arthropathy
- Farxiga®
- Flu - Influenza
- Fluoroscopy
- Gabapentin
- GERD
- Glycemic Index
- Gout
- Headaches
- Healing & Energy Work
- Health Facts
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Imaging Tests
- Herbal Terms
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- HIPAA
- Home Remedies
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hyperkalemia
- Hyperlipidemia
- Hypertension
- Hypoglycemia
- Hypokalemia
- Hypotension
- Important Numbers
- Indomethacin
- Informed Consent
- Inhalers
- Insomnia
- Insulin
- Juice Fasting
- Juice Recipes
- Kidney Cysts
- Kidney Disease
- Lantus®
- Lemon Benefits
- Lime Benefits
- Liver Disease
- Lumbar Retrolisthesis
- Medicaid
- Medical Specialties
- Medicare
- Medicare - Your Rights
- Melatonin
- Men's Health
- Mental Health
- MO HealthNet
- Mounjaro®
- MRI Scan
- Myelography
- Naproxen
- Nasal Polyps
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- Otolaryngologist
- Oxycodone-Acetaminophen
- Pain Management
- Peripheral Artery Disease
- Parking Spaces
- PET/CT Scan
- PET Scan
- Potassium
- Prescription Drugs
- Prurigo Nodularis
- PVC's
- Quetiapine
- Quit Smoking
- Radiculopathy
- Red Yeast Rice
- Reiki
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- SPECT Scan
- Spinal Stenosis
- Statins
- Stents
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Support Groups
- Tardive Dyskinesia
- Testosterone
- Trazodone
- Ultrasound
- Vaccines 19 and up
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin F
- Vitamin K
- Vitamins and Minerals
- Vitamins Recommended
- Water Benefits
- X-Rays
Needed to read PDF's
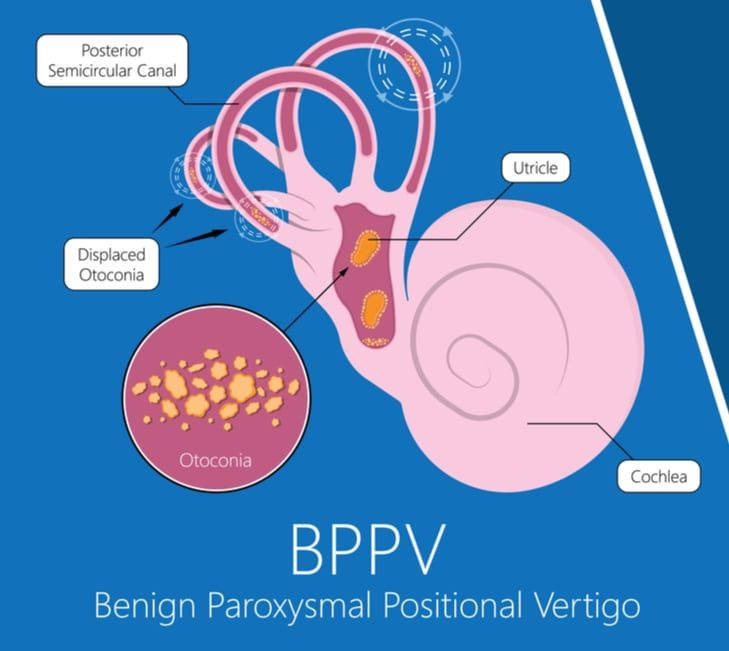
Benign Paroxysmal Positional Vertigo
(BPPV)
Overview
Benign paroxysmal positional vertigo (BPPV) is one of the most common causes of vertigo — the sudden sensation that you're spinning or that the inside of your head is spinning.
BPPV causes brief episodes of mild to intense dizziness. It is usually triggered by specific changes in your head's position. This might occur when you tip your head up or down, when you lie down, or when you turn over or sit up in bed.
Although BPPV can be bothersome, it's rarely serious except when it increases the chance of falls. You can receive effective treatment for BPPV during a doctor's office visit.
What is benign paroxysmal positional vertigo (BPPV)?
Benign paroxysmal positional vertigo (BPPV) is a common inner ear disorder. With BPPV, changes in your head position — such as tipping your head backward or sitting up in bed — lead to sudden vertigo (a feeling that the room is spinning).
BPPV isn’t a sign of a serious problem, and it usually disappears on its own within a few days of the first episode. (It could take several weeks for some people.) However, the symptoms of BPPV can be very frightening and may be dangerous, especially in adults over the age of 65. The unsteadiness of BPPV can lead to falls, which are a leading cause of fractures.
Who does benign paroxysmal positional vertigo affect?
BPPV can affect people of all ages, but it’s most common in adults over the age of 50. About half of all people in this age range experience at least one episode of BPPV in their lifetime.
BPPV can affect children, but it’s rare.
How common is BPPV?
Benign paroxysmal positional vertigo is the most common inner ear disorder. In fact, approximately 20% of people who are evaluated for dizziness are diagnosed with BPPV.
Is BPPV permanent?
BPPV usually goes away on its own. However, until it’s successfully treated, it can come back. In some cases, months — or even years — go by before another episode occurs.
Symptoms and Causes
What are the symptoms of benign paroxysmal positional vertigo?
Vertigo is the main symptom of BPPV. This vertigo sensation can range from mild to severe and may last seconds, or up to 1 minute.
It may be accompanied by other benign paroxysmal positional vertigo symptoms, including:
- Dizziness.
- Lightheadedness.
- Balance problems.
- Nausea and vomiting.
- Blurred vision.
- Nystagmus (rapid, involuntary eye movements). During a vertigo episode, patients with BPPV often exhibit nystagmus. This is involuntary eye movement. These movements are usually rotary or upbeat. They can help healthcare providers diagnose the affected ear and the specific semicircular canal involved.
While BPPV usually only affects one ear at a time, it can potentially affect both ears.
What triggers BPPV?
BPPV is almost always triggered by a change in your head’s position.
Vertigo episodes in BPPV are usually triggered by specific head movements. For example:
| Triggering Movement | Description |
| Rolling over in bed | Turning the head to one side while lying down |
| Looking up or down | Tilting the head back or forward |
| Bending over | Lowering the head, such as to pick something up |
| Getting in or out of bed | Transitions between lying down and sitting up |
In some instances, BPPV may be a symptom of another inner ear condition, such as:
- Labyrinthitis.
- Vestibular neuritis.
- Acoustic neuroma.
Additionally, BPPV may accompany migraines, or it may develop after a traumatic event — such as a fall, accident or sports injury.
Causes
The exact cause of BPPV is not always known. There are two main theories: canalithiasis and cupulolithiasis. Both involve tiny calcium carbonate crystals, called otoconia, moving in the inner ear.
Canalithiasis
Canalithiasis is the most common reason for BPPV. It happens when otoconia move from the utricle to a semicircular canal, often the posterior one. When the head moves, the otoconia cause the cupula to send false signals to the brain, leading to vertigo.
Cupulolithiasis
Cupulolithiasis is less common than canalithiasis. Here, otoconia stick to the cupula, the sensory part of the semicircular canal. This makes the cupula send false signals to the brain when the head moves, causing vertigo.
What brings on BPPV?
In many people, especially older adults, there is no specific event that causes BPPV to occur, but there are some things that may bring on an attack:
- Head trauma: A big hit to the head can knock otoconia loose, causing BPPV.
- Age: Older adults, over 50, are more likely to get BPPV because of natural changes in the otoconia.
- Osteoporosis: This condition can make otoconia more likely to move.
- Migraine: People with migraines are more likely to get BPPV, but why is not fully understood.
- Other things, like long bed rest, inner ear problems, and some medicines, can also lead to BPPV. Knowing these causes and risk factors helps in preventing and managing this common disorder.
Diagnosis and Tests
Your doctor may do a series of tests to determine the cause of your dizziness. During a physical exam, your doctor will likely look for:
- Signs and symptoms of dizziness that are prompted by eye or head movements and then decrease in less than one minute
- Dizziness with specific eye movements that occur when you lie on your back with your head turned to one side and tipped slightly over the edge of the examination bed
- Involuntary movements of your eyes from side to side
- Inability to control your eye movements
If your doctor can't find the cause of your signs and symptoms, he or she may order additional testing, such as:
- Electronystagmography (ENG) or videonystagmography (VNG). The purpose of these tests is to detect abnormal eye movement. ENG (which uses electrodes) or VNG (which uses small cameras) can help determine if dizziness is due to inner ear disease by measuring involuntary eye movements while your head is placed in different positions or your balance organs are stimulated with water or air.
- Magnetic resonance imaging (MRI). This test uses a magnetic field and radio waves to create cross-sectional images of your head and body. Your doctor can use these images to identify and diagnose a range of conditions. MRI may be performed to rule out other possible causes of vertigo.
Management and Treatment
There are several effective ways to manage benign paroxysmal positional vertigo (BPPV). The main goal is to ease symptoms and improve life quality. Common treatments include canalith repositioning maneuvers, vestibular rehabilitation therapy, and medications.
Canalith repositioning maneuvers, like the Epley maneuver, help move otoconia crystals back to the utricle. A healthcare professional guides these head and body movements. The choice of maneuver depends on the affected canal and BPPV type.
Vestibular rehabilitation therapy is key in BPPV treatment. It involves exercises to adapt to vestibular system changes. Patients learn head and eye movements to improve balance and reduce dizziness. This therapy is often paired with canalith repositioning maneuvers for best results.
Canalith Repositioning Maneuvers
Canalith repositioning maneuvers are a top choice for treating BPPV. They aim to move the otolith crystals back to the utricle. This helps get rid of vertigo and dizziness caused by BPPV.
Epley Maneuver
The Epley maneuver is a key method for BPPV in the posterior semicircular canal. It involves head movements to move the crystals back to the utricle. A healthcare pro does this, but you can also learn it at home.
Semont Maneuver
The Semont maneuver is great for BPPV in the posterior semicircular canal. It involves quick side-to-side movements with the head up. This helps move the crystals back to the utricle.
Foster Maneuver
The Foster maneuver, or half somersault, is a home treatment for BPPV in the posterior semicircular canal. It’s done by following specific head and body movements. It’s an option instead of the Epley and Semont maneuvers.
Here are the success rates of these maneuvers:
| Maneuver | Success Rate |
| Epley | 80-90% |
| Semont | 75-85% |
| Foster | 70-80% |
Some patients might need more than one session to fully get rid of BPPV symptoms. Always talk to a healthcare pro before trying these at home. They can guide you and make sure you’re doing it right.
Vestibular Rehabilitation Therapy
Vestibular rehabilitation therapy is a special kind of physical therapy. It helps people with BPPV get better at balancing and feeling stable. This therapy includes three main types of exercises: balance, gaze stabilization, and habituation.
Balance exercises help you stay steady and avoid falls. You might stand on different surfaces, walk heel-to-toe, or do single-leg stands. These exercises help your brain learn to keep you stable again.
Gaze stabilization exercises improve how your eyes and brain work together. They reduce vertigo and dizziness from BPPV. You’ll focus on a fixed object while moving your head or track a moving object with your eyes.
Habituation exercises help you get used to things that usually make your BPPV symptoms worse. By facing these triggers in a safe way, you can make your symptoms less severe. For example, the Brandt-Daroff exercises help your brain adjust to position changes.
Your physical therapist will create a plan just for you. They’ll consider your needs and how bad your symptoms are. With regular practice and your therapist’s help, you can manage your symptoms and live better.
What is the fastest way to cure BPPV?
The most effective benign paroxysmal positional vertigo treatments involve physical therapy exercises. The goal of these exercises is to move the calcium carbonate particles out of your semicircular canals and back into your utricle. Here, the particles resorb more easily and don’t cause uncomfortable symptoms.
You can also take motion sickness medications to relieve your symptoms. However, you shouldn’t take these medications long term.
Benign paroxysmal positional vertigo exercises: How do they work?
Vertigo is often caused by the displacement of small calcium carbonate crystals, or canaliths, within your inner ear. The Epley maneuver, also known as the canalith repositioning procedure (CRP) is a method to remove these crystals trapped in your ear’s semicircular canal. typically take about 15 minutes to complete. Particle repositioning involves a series of physical movements that change the position of your head and body. These actions shift the otoconia out of your semicircular canals and back into their proper location in your utricle.
A single particle repositioning procedure is effective in treating about 80% to 90% of cases of BPPV. Additional BPPV exercises may be needed if symptoms continue.
Your healthcare provider can perform this maneuver during an office visit. They can also demonstrate how to do these exercises at home to ease your BPPV symptoms.
In the meantime, here are some step-by-step instructions to try:
- Step 1: Start by sitting up on a bed or table. Turn your head 45 degrees toward the affected ear.
- Step 2: Quickly lie back, keeping your head turned toward the affected ear as you lie back with your head slightly over the edge of the bed or table. Wait about a minute or until you stop having symptoms.
- Step 3: Without raising your head, turn your head quickly in the opposite direction so that your “good” ear is parallel with — but slightly over the edge of — the table or bed. Wait about a minute or until you stop having symptoms.
- Step 4: Roll onto your side. Continue to turn your head another 90 degrees in the same direction as step 3 so that your nose is now facing the floor. Wait about a minute.
- Step 5: Keeping your chin tucked in toward your shoulder, sit up in the direction your body is facing. Follow any post-particle repositioning instructions given to you by your healthcare provider.
Surgical alternative
In rare situations when the canalith repositioning procedure doesn't work, your doctor may recommend a surgical procedure. In this procedure, a bone plug is used to block the portion of your inner ear that's causing dizziness. The plug prevents the semicircular canal in your ear from being able to respond to particle movements or head movements in general. The success rate for canal plugging surgery is about 90%.
What Are Benign Paroxysmal Positional Vertigo (BPPV) Medications?
Several medications, including common motion sickness remedies, may relieve symptoms of BPPV and may be used for less severe episodes of vertigo or in addition to the Epley maneuvers described above.
- meclizine (Antivert, Bonine, Dramamine II, D-Vert)
- diazepam (Valium)
- dimenhydrinate (Dramamine)
- promethazine (Phenergan)
- scopolamine (Isopto, Scopace)
If the cause of vertigo is thought to be due to a viral infection, antiviral medications like acyclovir (Zovirax) may be prescribed.
Steroids like prednisone may be useful if nerve inflammation is a potential reason for vertigo.
Can BPPV go away on its own?
Yes. In many cases, BPPV goes away on its own eventually. But it can come back. If it does, your healthcare provider can tell you how to manage your symptoms when they occur.
Lifestyle and home remedies
Coping with Benign Paroxysmal Positional Vertigo (BPPV) can be tough. But, there are ways to manage your symptoms and live better. By changing your daily routine and home, you can lessen BPPV’s effects on your life.
Adapting daily activities
To cut down vertigo episodes, adjust your daily life. Move slowly when changing positions, like getting out of bed. Avoid quick head movements and bending or looking up. Use extra pillows at night to keep your head up and prevent vertigo.
Fall prevention strategies
Falls are a big worry for BPPV sufferers. To lower this risk, make your home safer. Put handrails on stairs and in bathrooms, remove tripping hazards, and brighten your home. Use a cane or walker for extra support. These steps can help you stay safe and independent.
If you experience dizziness associated with BPPV, consider these tips:
- Be aware of the possibility of losing your balance, which can lead to falling and serious injury.
- Avoid movements, such as looking up, that bring on the symptoms.
- Sit down immediately when you feel dizzy.
- Use good lighting if you get up at night.
- Walk with a cane for stability if you're at risk of falling.
- Work closely with your doctor to manage your symptoms effectively.
BPPV may recur even after successful therapy. Although there's no cure, the condition can be managed with physical therapy and home treatments.
How can I reduce my risk for BPPV?
You can’t prevent BPPV, but you can manage it with particle repositioning exercises. To reduce your risk of trauma-related BPPV, be sure to wear a helmet when biking, playing contact sports or participating in other similar activities.
Prognosis
What can I expect if I have benign paroxysmal positional vertigo?
The good news is that BPPV doesn’t indicate a serious health problem. Even so, dealing with your symptoms can be scary and frustrating. Your healthcare provider can teach you how to do BPPV exercises at home so you can manage your symptoms at the first sign of trouble.
How long does BPPV last?
In most cases, a BPPV episode lasts 1 to 2 minutes. Your symptoms may be mild, or they may be so severe that you throw up. You might even lose your balance when you try to stand or walk.
Can Benign Paroxysmal Positional Vertigo (BPPV) Go Away on Its Own?
BPPV usually resolves on its own quickly or within a few weeks or months, even without any specific treatment.
- The Epley maneuver may cure the problem immediately.
- Medications may help control the severity of symptoms
- Vertigo may recur months or years later after an initial incidence.
- BPPV is rarely a problem that cannot be resolved. Neurologists, otolaryngologist, and vestibular rehabilitation physical therapists may be of help in confirming the diagnosis and resolving BPPV or controlling its symptoms.
When should I call the doctor?
Make an appointment with your doctor if you have symptoms common to BPPV. After an initial examination, your doctor may refer you to an ear, nose and throat (ENT) specialist or a doctor who specializes in the brain and nervous system (neurologist).
Here's some information to help you get ready for your appointment.
What you can do
- Write down your symptoms, including when they started and how often they occur.
- Note any recent blows to your head, including even minor accidents or injuries.
- Make a list of your key medical information, including any other conditions for which you're being treated and the names of any medications, Vitamins and supplements you're taking.
- Write down questions to ask your doctor. Creating your list of questions can help you make the most of your time with your doctor.
Questions to ask the doctor at the initial appointment include:
- What are the possible causes of my symptoms or condition?
- What tests do you recommend?
- If these tests don't pinpoint the cause of my symptoms, what additional tests might I need?
- Do I need to follow any restrictions while waiting for a diagnosis?
- Should I see a specialist?
Questions to ask if you are referred to a specialist include:
- What treatments are most likely to help me feel better?
- How soon after beginning treatment should my symptoms start to improve?
- If the first treatment doesn't work, what will you recommend next?
- Am I a candidate for surgery? Why or why not?
- What self-care steps can help me manage this condition?
- Do I need to restrict my activities? For how long?
- Am I at risk of this problem recurring?
- I have these other health conditions. How can I manage these conditions together?
- What handouts or websites do you recommend for learning more about BPPV?
What to expect from your doctor
A doctor who sees you for symptoms common to BPPV may ask a number of questions, such as:
- What are your symptoms, and when did you first notice them?
- Do your symptoms come and go? How often?
- How long do your symptoms last?
- Does anything in particular seem to trigger your symptoms, such as certain types of movement or activity?
- Do your symptoms include vision problems?
- Do your symptoms include nausea or vomiting?
- Do your symptoms include headache?
- Have you lost any hearing?
- Are you being treated for any other medical conditions?
Seek Emergency Care
Although it's uncommon for dizziness to signal a serious illness, see your doctor immediately if you experience dizziness or vertigo along with any of the following:
- A new, different or severe headache
- A fever
- Double vision or loss of vision
- Hearing loss
- Trouble speaking
- Leg or arm weakness
- Loss of consciousness
- Falling or difficulty walking
- Numbness or tingling
The signs and symptoms listed above may signal a more serious problem.
Benign Paroxysmal Positional Vertigo (BPPV) Terms
- Semicircular canals: These structures act like a gyroscope, with canals positioned in three dimensions: upward, downward, and horizontal. Together, the canals send signals to your brain about the rotation/positioning of your head (for example, when you bend over or spin around.)
- Cupula: Detects the flow of fluid within your semicircular canals. The flow of fluid gives your body a sense of motion.
- Utricle: An organ located in your inner ear that helps control balance. Your utricle contains hair cells, which are covered with otoconia. The otoconia sway with gravity, sending signals to your brain about the position of your head and body (upright, tilted, etc.).
- Otoconia: The tiny calcium crystal particles that become dislodged from within your utricle (where they can dissolve) and move into your semicircular canals (where they can’t dissolve).
- Cochlea: The “snail-shell” sense organ of your inner ear that translates sound into nerve impulses that are sent to your brain.
FAQ's
Q: What is Benign Paroxysmal Positional Vertigo (BPPV)?
A: BPPV is a common disorder that causes brief dizziness. It happens when tiny crystals in the inner ear move. This movement can cause a spinning feeling when you move your head.
Q: What are the symptoms of BPPV?
A: BPPV makes you feel dizzy when you move your head. This can happen when you look up or roll over in bed. You might also feel sick, vomit, or have trouble balancing.
Q: How is BPPV diagnosed?
A: Doctors use special tests to find BPPV. These tests move your head in certain ways. They look for signs of dizziness and eye movements. This helps rule out other problems.
Q: What causes BPPV?
A: BPPV is caused by crystals moving in the inner ear. This can happen from a head injury, getting older, or other ear issues. There are two main reasons for this movement.
Q: What are the treatment options for BPPV?
A: Treatments for BPPV include special head movements and therapy. These help move the crystals back to where they belong. Therapy also helps you get used to the symptoms and balance better.
Q: Can BPPV resolve on its own?
A: Sometimes, BPPV goes away by itself. But, it’s important to see a doctor. They can help figure out what’s wrong and treat it to make you feel better.
Q: How can I manage BPPV in daily life?
A: To deal with BPPV, you might need to change how you do things. You could make your home safer, use special tools, or learn how to prevent falls. Your doctor can help you find ways to live better with BPPV.
One Final Note..
Benign paroxysmal positional vertigo isn’t life-threatening, but it can have a significant negative impact on your quality of life. If you’ve experienced sudden episodes of dizziness, vertigo, balance problems or other symptoms related to BPPV, call your healthcare provider. In most cases, physical therapy exercises and home treatments can keep your symptoms at bay.
The lifetime prevalence of BPPV is about 2.4% and other estimates range from 10-64 per 100,000 people in the general population. However, many physicians think that the true frequency may be higher. BPPV most often affects older adults with a peak age of onset in the sixth decade. The disorder may affect individuals of any age but is quite uncommon in those under 20 years of age. Females are thought to be affected at least twice as often as males.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 - K. Kerr Most recent revision February 09, 2026 07:44:16 AM
|











