- Main Page
- A1C Test
- Advance Directives
- Anxiety
- Aortic Aneurysm
- Aphrodisiacs
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation - AFib
- Back Pain
- Blood Tests
- Blood Test Tubes
- Blood Types
- BMI Calculator
- Body Mass Index - BMI
- Bone Density Scan
- Bone Scan
- BPPV
- Bronchitis
- Cancer - Lung
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- Caregiver Glossary
- Caregiver Resources - LGBTQ+
- Caregiver Resources - MO
- Caregiver Resources - USA
- Continuous Glucose Monitors
- Cholesterol
- Citalopram
- COPD
- Coronary Artery Disease
- Cough
- CPAP
- CT scan
- Cyclobenzaprine
- Degenerative Disc Disease
- Depression
- Diabetes Information
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes Facts
- Diabetes Care
- Diabetes Care Team
- Diabetes & Fruits
- Diabetes - Gestational
- Diabetes - Pre
- Diabetic Terms
- Diabetes & Vegetables
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Disability Permits
- Do Not Resuscitate
- Dupixent®
- Echocardiogram
- E-Cigarettes
- Electrocardiogram
- Electromyography
- Emphysema
- Epidural - Lumbar
- Epidural - Transforaminal
- Epsom Salt
- Facet Arthropathy
- Farxiga®
- Flu - Influenza
- Fluoroscopy
- Gabapentin
- GERD
- Glycemic Index
- Gout
- Headaches
- Healing & Energy Work
- Health Facts
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Imaging Tests
- Herbal Terms
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- HIPAA
- Home Remedies
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hyperkalemia
- Hyperlipidemia
- Hypertension
- Hypoglycemia
- Hypokalemia
- Hypotension
- Important Numbers
- Indomethacin
- Informed Consent
- Inhalers
- Insomnia
- Insulin
- Juice Fasting
- Juice Recipes
- Kidney Cysts
- Kidney Disease
- Lantus®
- Lemon Benefits
- Lime Benefits
- Liver Disease
- Lumbar Retrolisthesis
- Medicaid
- Medical Specialties
- Medicare
- Medicare - Your Rights
- Melatonin
- Men's Health
- Mental Health
- MO HealthNet
- Mounjaro®
- MRI Scan
- Myelography
- Naproxen
- Nasal Polyps
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- Otolaryngologist
- Oxycodone-Acetaminophen
- Pain Management
- Peripheral Artery Disease
- Parking Spaces
- PET/CT Scan
- PET Scan
- Potassium
- Prescription Drugs
- Prurigo Nodularis
- PVC's
- Quetiapine
- Quit Smoking
- Radiculopathy
- Red Yeast Rice
- Reiki
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- SPECT Scan
- Spinal Stenosis
- Statins
- Stents
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Support Groups
- Tardive Dyskinesia
- Testosterone
- Trazodone
- Ultrasound
- Vaccines 19 and up
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin F
- Vitamin K
- Vitamins and Minerals
- Vitamins Recommended
- Water Benefits
- X-Rays
Needed to read PDF's
Stents
What Are Stents?
A stent is a small mesh tube typically used to hold open passages in the body, such as weak or narrowed blood vessels. Stents are often used to treat narrowing in the coronary arteries, which provide the heart with oxygen-rich blood. Stents can also help to treat an aneurysm, which is a bulge in the wall of an artery, as well as narrowed airways in the lungs.
Stenting is a minimally invasive procedure, meaning it does not require a large, open incision in the body and is not considered major surgery. However, before you get a stent, you may need certain tests or some medicines to prepare for the procedure. Stents can be made of metal mesh, fabric, silicone, or combinations of materials. Stents for coronary arteries are usually made of metal mesh and sometimes covered with another material. Fabric stents, or stent grafts, are used in larger arteries such as the aorta. Stents used in the airways of the lungs are often made of silicone.
After you receive a stent, and depending on its location in the body, you may need to take certain medicines, such as aspirin and other antiplatelet medicines that prevent your blood from forming clots. Your healthcare provider may recommend taking this medicine for a year or longer after receiving an artery stent to prevent complications. The most common problems are a stent becoming blocked, a blood clot forming in an artery stent, or an airway stent moving out of place.
Types of stents
Stents have different purposes. The materials used in stents can vary depending on where they will go in the body.
Airway stents
Some stents are used in the airways in the lungs. Airway stents are usually temporary.
- Metal stents are made of bare metal or covered with another material, such as silicone. They can be difficult to remove from the airways, so they are not common.
- Silicone stents are made of a material that can be molded to a certain shape. They are more common, because they are easy to insert and remove. Some silicone stents are 3D printed and can be custom fit for each person.
Vascular Stents: Applications Beyond the Heart
Vascular stents are not just for the heart. They help treat many blood vessel issues across the body. These devices improve blood flow and prevent serious problems.
They are often used for peripheral artery disease (PAD). PAD happens when arteries in the legs or arms get narrow or blocked. This reduces blood flow and causes pain, numbness, and weakness. A vascular stent can fix this by opening up the artery.
Vascular stents also help with carotid artery stenosis. The carotid arteries in the neck supply blood to the brain. If these arteries narrow or block, stroke risk goes up. A stent in the artery can widen it, improving blood flow and lowering stroke risk.
Aortic aneurysm stents
Stent grafts are used to treat aortic aneurysms. The stent graft is typically a tube made of leak proof polyester with metal mesh underneath. Stent grafts are used in larger arteries, such as the aorta, and provide a stable channel for the blood to flow through.
Coronary or carotid artery stents
Cardiac stents are key in treating coronary artery disease. This disease narrows or blocks arteries that supply blood to the heart. The buildup of plaque causes this narrowing, restricting blood flow and leading to serious health issues.
- Bare metal stents : Advantages and Disadvantages
Bare-metal stents are made of a mesh-like metal framework. They help keep the artery open after angioplasty. The benefits include:
- Lower cost compared to drug-eluting stents
- Shorter duration of blood-thinning medication required post-procedure
- Suitable for patients who may not tolerate long-term blood-thinning medication
But, bare-metal stents also have some downsides:
- Higher risk of stent restenosis (re-narrowing of the artery) compared to drug-eluting stents
- May require additional procedures if restenosis occurs
- Biodegradable stents are temporary and dissolve after a few months.
- Drug-eluting stents : Advantages and Disadvantages
Drug-eluting stents are coated with a slow-release medication. This helps prevent scar tissue formation and reduces the risk of stent restenosis.
The benefits include:
- Lower risk of restenosis compared to bare-metal stents
- Reduced need for repeat procedures
- Improved long-term outcomes for patients
But, drug-eluting stents also have some drawbacks:
- Higher cost compared to bare-metal stents
- Longer duration of blood-thinning medication required post-procedure (usually 6-12 months)
- Slightly higher risk of late stent thrombosis (blood clot formation) compared to bare-metal stents
The choice between a bare-metal stent and a drug-eluting stent depends on several factors. These include the patient’s health condition, risk factors, and the location and severity of the blockage. The following table compares the key features of bare-metal and drug-eluting stents:
How Stents Work in the Body
Stents are tiny mesh tubes that help treat narrowed or blocked arteries. They are key for those with coronary artery disease. These devices restore blood flow and support the artery walls, improving blood vessel health.
Mechanism of Action
A stent is placed in a narrowed or blocked artery during angioplasty. It is expanded, pushing plaque against the wall. This creates a wider opening for blood flow. The stent stays in the artery, keeping it open and preventing future blockages.
Benefits of Stent Implantation
Stent implantation brings many benefits for patients with coronary artery disease and other vascular conditions:
- Improves blood flow to the heart and other vital organs
- Relieves symptoms such as chest pain (angina) and shortness of breath
- Reduces the risk of heart attack and stroke
- Minimizes the need for more invasive surgical procedures, such as coronary artery bypass grafting (CABG)
- Enables quicker recovery times compared to open heart surgery
Stents restore blood flow and support artery walls. This improves life quality for patients with cardiovascular conditions. It lets them return to daily activities with more ease and confidence.
When Do You Need a Stent?
Your healthcare provider may recommend a stent to support a narrow or weak artery or airway. They will discuss the risks and benefits with you. Several conditions may lead your provider to recommend a stent.
Aortic aneurysm or dissection
Your healthcare provider may use a stent graft to treat an aneurysm or dissection of the aorta, the main artery carrying oxygen-rich blood to your body. Some medical conditions can damage the walls of the aorta. When the walls are weak, the force of the blood pushing through can cause an aneurysm or balloon-like bulge in the aorta. The stent graft supports the weak area of the aorta and helps to prevent the aneurysm from bursting or tearing the wall of the artery (dissection). Stent grafts can also help control blood flow after an injury and stop blood from leaking out of the blood vessel and into the body.
Coronary Artery Disease
Stents are often used to treat narrowed coronary arteries. In coronary heart disease, the arteries cannot carry enough oxygen-rich blood to the heart. Low blood flow to the heart can lead to chest pain and damage to the heart muscle from a heart attack.
To understand the causes of Coronary Artery Disease, it helps to learn about how the heart works.
Carotid artery disease
The carotid arteries are arteries in the neck that carry oxygen-rich blood to the brain. Plaque buildup in the carotid arteries can cause carotid artery disease and increase the risk of stroke. Placing a stent in a narrowed carotid artery can help hold the artery open and restore normal blood flow to the brain.
Peripheral artery disease
In peripheral artery disease, plaque builds up in the arteries that carry blood to your legs, arms, or abdomen. Stents can help treat the narrowed arteries, relieve symptoms, and prevent future health problems that can result from low blood flow.
Lung conditions
Stents can help treat narrowed airways in the lungs. Unlike stents for arteries, airway stents are usually a temporary solution before surgery or other more permanent treatments. Silicone stents are easy to move or remove from the airways and can remain in place for several years. Metal stents, on the other hand, are harder to remove the longer they stay in the airway, so they are less commonly used.
There are different reasons why someone may need an airway stent.
- Problems you are born with, also called congenital conditions, may create the need for an airway stent.
- Infections or conditions such as sarcoidosis can cause swelling that squeezes the airways. Anything that presses on the lungs can cause the airways to become narrowed or blocked.
- Injury to the airways can occur from intubation, which is performed when a breathing tube is guided down into the lungs to help you breathe. Damage from some lung treatments can also lead to narrowed airways, such as from a tracheostomy or if a hole forms where transplanted lungs were stitched together.
- Tumors can block the airways. Cancer treatment, such as radiation or chemotherapy, can sometimes damage the airways too.
To understand the airways, it helps to learn more about how the lungs work.
What are the complications associated with inserting a stent?
Any surgical procedure carries risks. Inserting a stent may require accessing arteries of the heart or brain. This leads to an increased risk of adverse effects.
The risks associated with stenting include:
- an allergic reaction to medications or dyes used in the procedure
- breathing problems due to anesthesia or using a stent in the bronchi
- bleeding
- a blockage of the artery
- blood clots
- a heart attack
- an infection of the vessel
- kidney stones due to using a stent in the ureters
- a re-narrowing of the artery
Rare side effects include strokes and seizures.
Few complications have been reported with stents, but there’s a slight chance the body will reject the stent. This risk should be discussed with your doctor. Stents have metal components, and some people are allergic or sensitive to metals. Stent manufacturers recommend that if anyone has a sensitivity to metal, they should not receive a stent. Speak with your doctor for more information.
If you have bleeding issues, you will need to be evaluated by your doctor. In general, you should discuss these issues with your doctor. They can give you the most current information related to your personal concerns.
More often than not, the risks of not getting a stent outweigh the risks associated with getting one. Limited blood flow or blocked vessels can create serious and deadly consequences.
When a stent may not be recommended
Your healthcare provider will consider your health, talk to you about the risks, and help you make a decision.
An artery stent may not be recommended if:
- Your condition is mild. Your provider may monitor your condition, start you on medicine, and recommend heart-healthy lifestyle changes.
- You cannot take antiplatelet medicines for the amount of time needed after the stenting procedure. Antiplatelet medicines prevent the formation of life-threatening blood clots inside the stent.
- You have other medical conditions, such as multiple narrowed coronary arteries, long-standing kidney disease, or diabetes. Your provider may recommend coronary artery bypass graft surgery (CABG) instead.
- You have a high risk for complications. Age or other risk factors may lead your provider to recommend a different treatment instead of a carotid stent, especially if you are over age 70 or you have a high risk of stroke. Stent grafts may be riskier for older people and those with conditions such as kidney or heart failure.
An airway stent may not be recommended if:
- You cannot have anesthesia or be sedated.
- You need other procedures in the future, such as laser therapy, which can break or burn the stent. An airway stent can also get in the way if you need lung surgery for other reasons.
Before You Get a Stent
Your healthcare provider can help decide whether you need a stent by using certain tests and procedures. If you need a stent, your provider will talk to you about how to prepare for it.
Diagnostic tests and procedures
To diagnose narrowed arteries or an aortic aneurysm, your provider may order some of the following heart tests and procedures.
- Chest magnetic resonance imaging (MRI) looks for aneurysms in the aorta. This test works well to find aneurysms and pinpoint their size and exact location.
- Computed tomography angiography (CTA) and magnetic resonance angiography (MRA) take pictures of your blood vessels. These tests may give your provider more information about blood flow and whether arteries are narrowed or have aneurysms.
- Coronary angiography measures how blood flows through your coronary arteries. This type of test involves injecting dye into your blood so that your blood vessels can be seen by X-ray.
- Fractional flow reserve can help determine how narrow the artery is. This is an added test done during CTA or coronary angiography to check the blood pressure, or how much force is needed for the blood to flow through the artery.
- Ultrasound looks at whether plaque has narrowed or blocked your carotid or peripheral arteries. It is also used to see whether you have an aneurysm and where it is located. This painless test uses high-energy sound waves to create pictures of the insides of your blood vessels.
- Echocardiography (echo or ECG) evaluates the structure and function of your heart, using sound waves to create moving pictures.
- Nuclear imaging checks whether the blood is flowing normally to the heart. Your provider will inject a substance they can trace through your bloodstream to see whether the heart is receiving enough blood flow.
To diagnose narrowed airways, you may need some lung tests and procedures.
- Bronchoscopy determines the location and severity of the narrowed airway.
- Chest computed tomography (CT) scans look at whether one of your airways is being affected by a tumor, pneumonia, mucus, or other problem.
- Lung spirometry tests measure how well your lungs are working.
Preparing for the stenting procedure
You may need more tests, such as blood tests and electrocardiogram, chest X-ray, or chest CT scans, to prepare for the procedure to place a stent. Tell your provider about medicines you take, other surgical procedures you have had, and any medical conditions, such as diabetes, kidney disease, or sleep apnea.
You will be asleep for most stent procedures, so plan to have someone else take you home afterward. You may go home the same day or after a few days, depending on the type of stent and your other medical conditions.
Before your procedure, you will be given detailed information, including:
- When to stop eating or drinking
- If and when you should start or stop taking medicines
- When to arrive at the hospital and where to go
- How long you should expect to stay
- What happens during the procedure
- What to expect after the procedure, including potential complications such as bleeding or soreness
- What to do after the procedure, including what medicines to take
- How to live with your stent(s)
Getting a Stent
Having a stent placed is a minimally invasive procedure, meaning it does not require a large open incision.
Coronary and carotid artery stenting
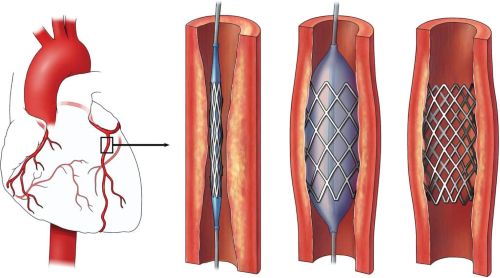
Procedures to place a stent to treat coronary and carotid arteries are similar. In both, your healthcare provider will use catheterization to thread a thin tube with a stent and an empty balloon on the end through the blood vessel to the narrowed or blocked artery. Once the balloon is in place, filling it with air opens the stent to hold up the artery walls. Then your provider will empty the balloon of air again and remove the tube and the empty balloon from the artery.
- Percutaneous coronary intervention (PCI). or coronary angioplasty, opens narrowed or blocked arteries of the heart to treat coronary heart disease. A coronary stent can be placed during a PCI to prevent the artery from narrowing again. Sometimes the procedure is done in an emergency, such as during a heart attack.
Placing a stent in a narrowed coronary artery. The coronary arteries surround the heart and provide oxygen-rich blood to the heart muscle. To place a stent in a coronary artery narrowed by plaque, a catheter is inserted with an empty balloon and a stent attached at the end. The balloon is inflated to push the artery open and open the stent. Finally, the catheter and balloon are removed, leaving the stent in place to keep the artery open and prevent it from narrowing again.
- Carotid artery stenting. is a minimally invasive treatment for severe carotid artery disease. Usually, the procedure to place a carotid stent includes temporarily blocking the blood flow from the narrowed artery to the brain. This helps prevent any pieces of plaque from reaching the brain and causing a stroke.
Placing a stent in a narrowed carotid artery in the neck. The carotid arteries carry oxygen-rich blood to the brain. To place a stent in a carotid artery narrowed with plaque, a catheter is inserted with a stent and an empty balloon at the end. In the narrowed area, the balloon is filled with air to widen the artery and open the stent in place. After the catheter and balloon are removed, the expanded stent helps keep the artery open to restore normal blood flow to the brain.
Aortic aneurysm stenting
The procedure to place a stent graft in the aorta to treat an aneurysm is called endovascular aneurysm repair. Your healthcare provider inserts a stent graft through a large blood vessel using a catheter and guides it up your arteries to the location of the aneurysm. Once it is in the right place, the stent graft opens up and attaches to the walls of the aorta. This will seal off the aneurysm and prevent it from getting bigger or rupturing. After placing the stent graft, your provider may inject a contrast dye into your blood and take an X-ray of your aorta to make sure blood is not leaking into the aneurysm.
Placing a stent graft in aortic aneurysm. A catheter is inserted into an artery through a small cut in the upper thigh. The catheter guides the stent graft to the abdominal aorta. At the aneurysm, the stent graft expands as the catheter is slowly pulled back out. Once the stent graft is in place, it allows blood to flow through the aorta without pushing against the aneurysm’s weak walls.
Airway stenting
Bronchoscopy uses a small camera on the end of a long tube to look inside the airways in your lungs. To do that, your healthcare provider slides the camera, or bronchoscope, through your nose or mouth and down your throat into the airways. During the procedure, your provider can also insert an airway stent or take samples for diagnostic tests.
If you need a stent, your provider will slide a thin tube that carries the folded stent along the side of the bronchoscope. Your provider may also use fluoroscopy, a type of X-ray imaging, or ultrasound to help guide stent placement. Once it is in the right area, the stent will expand in the narrowed airway to push it open. After placing the stent, your provider may check your lungs using a chest X-ray.
After You Get a Stent
Recovery
Before you leave the hospital, your healthcare provider will give you instructions to follow at home.
- Take your medicines according to your provider’s directions. You may need to take medicines to prevent complications. For example, antiplatelet medicines can help stop a blood clot from forming in a coronary stent.
- Resume normal physical activity and return to work when your provider says it’s okay. For most people, this can happen within a few days to a week.
- Make a follow-up appointment. Your provider will want to check on your progress and make sure there are no problems.
Risks and Complications Associated with Stents
Stents have greatly helped in treating heart and artery diseases. Yet, they come with risks. The main issues are stent thrombosis and stent restenosis.
Stent Thrombosis
Stent thrombosis happens when a blood clot blocks the stent. This can cause a heart attack or even death. Symptoms include chest pain, shortness of breath, and dizziness. Risks include:
| Risk Factor | Description |
| Premature discontinuation of antiplatelet therapy | Stopping prescribed medications too early after stent implantation |
| Stent underexpansion | Inadequate expansion of the stent during the procedure |
| Stent malapposition | Poor contact between the stent and the artery wall |
| Hypersensitivity reactions | Allergic reactions to stent materials or medications |
To lower stent thrombosis risk, follow your antiplatelet therapy. Also, keep up with your doctor’s appointments.
Stent Restenosis
Stent restenosis is when the artery narrows again. It often happens in the first few months. It can make symptoms come back. Risks include:
- Diabetes
- Longer lesions
- Smaller vessel diameter
- Inadequate stent expansion
For stent restenosis, treatments are available. These include repeat angioplasty or stent placement. Drug-eluting stents have lowered restenosis rates. But, regular checks are key for early detection.
Results
Coronary angioplasty and stent placement can greatly increase blood flow through a previously blocked or narrowed heart artery. Your doctor can compare images of your heart taken before and after the procedure to determine how well the angioplasty and stenting has worked.
Angioplasty with stenting does not treat the underlying causes of blockages in your arteries. To keep your heart healthy after angioplasty, try these tips:
- Do not smoke or use tobacco.
- Eat a diet that is low in saturated fats and rich in vegetables, fruits, whole grains, and healthy oils such as olive oil or avocado.
- Maintain a healthy weight. Ask a healthcare professional what a healthy weight is for you.
- Get regular exercise.
- Control cholesterol, blood pressure and blood sugar.
Living With a Stent
If you have a stent because of Coronary Artery Disease or carotid artery disease, you are still at risk of having a heart attack or a stroke. Learn the signs of a heart attack and the signs of a stroke and call 9–1–1 if you or someone else needs help.
Receive routine follow-up care
A stent is a treatment, but it cannot cure your underlying condition. It is important to have routine medical care if you have a stent. Ask your healthcare provider how often you should schedule office visits and tests.
- Talk about when to follow up with specialists such as a cardiologist or pulmonologist. If you have an airway stent, you may need a bronchoscopy, a chest X-ray, or a CT scan to confirm that the stent has not moved. These tests can also check for signs of complications. If you have a stent graft to treat an aortic aneurysm, you may need regular imaging tests for the rest of your life to make sure that there is no blood leaking into the aneurysm and to monitor your stent graft.
- Take medicines to prevent problems. Do not change your medicine or skip doses unless your provider tells you to. After getting an artery stent, you will need antiplatelet medicines, or blood thinners, to prevent blood clots from forming. You may need to take blood thinners for more than a month after you get a carotid or peripheral artery stent or for more than a year after getting a coronary stent. Antiplatelet medicines include aspirin, clopidogrel, dipyridamole, and ticlopidine. Bleeding is a possible side effect, which can make any other needed surgery much riskier.
- Ask how long before you can resume normal physical activity. It will depend on the type of stent you have and your health condition before the procedure.
Make healthy lifestyle changes
Your provider may recommend the following healthy lifestyle changes to lower your risk of needing future procedures or experiencing complications such as a heart attack or stroke:
- Aim for a healthy weight
- Stay physically active
- Choose heart-healthy foods
- Manage stress
- Quit smoking and avoid secondhand smoke
- Get enough good-quality sleep
Watch for problems from vascular stents
Be on the lookout for complications from a coronary stent, carotid stent, or stent graft.
- Blood clots can form within the stent. Your risk of getting a blood clot is much higher if you stop taking your blood thinners before your provider says to do so. Blood clots can lead to life-threatening conditions, such as heart attack, stroke, and venous thromboembolism.
- Restenosis is a re-narrowing of the section of the artery where there is a stent. The artery can become narrow again when there is too much tissue growth inside it. With a coronary stent, restenosis can lead to a heart attack. With a carotid stent, a stroke can occur. Restenosis may or may not cause symptoms. If it does occur, you may need a new stent or another procedure.
- A stent graft can leak or move from its place. Symptoms may be similar to those you experienced before the aortic repair procedure, or you may have no symptoms. Your provider will use imaging to monitor your stent graft.
Watch for problems from lung stents
Call your provider right away if you experience any of the following symptoms:
- Breathing problems
- Changes in your cough
- Coughing up blood
- High fever
- Persistent bad breath
Those symptoms may result from complications of your airway stent.
- An airway stent can migrate, or move, and may require another procedure to fix or remove it. This occurs more often with silicone stents.
- Lung infection is another possible complication from an airway stent.
- Mucus can get caught in the stent and block it.
- Tissue can grow into the stent if the condition that caused your narrowed airway causes it to become blocked again. This happens more often with metal stents.
Advances in Stent Technology
In recent years, stent technology has seen big improvements. These changes aim to make treatments better and safer for patients. The focus is on biodegradable stents and new stent coatings and materials.
Biodegradable Stents
Biodegradable stents are made to support arteries temporarily and then dissolve. They are made from materials like polylactic acid (PLA) or magnesium alloys. This design could offer several benefits, such as:
| Benefit | Description |
| Reduced long-term complications | As the stent dissolves, the risk of late stent thrombosis and restenosis is minimized |
| Restoration of natural vessel function | The artery can resume its normal vasomotion and adapt to future changes in blood flow |
| Improved future treatment options | Without a permanent implant, patients can undergo additional interventions if needed |
Stent Coatings and Materials
Scientists are also working on new stent coatings and materials. These innovations aim to make stents work better and be safer for the body. Some exciting developments include:
- Drug-eluting coatings: Advanced drug-eluting coatings can deliver medications more precisely and over an extended period, reducing the risk of restenosis and promoting faster healing
- Biocompatible materials: New stent materials, such as titanium-nitride-oxide and diamond-like carbon, are being investigated for their excellent biocompatibility and resistance to corrosion
- Nanostructured surfaces: Stents with nanostructured surfaces can promote endothelialization, the growth of a new, healthy lining in the artery, which helps prevent blood clots and restenosis
As research goes on, the mix of biodegradable stents and new coatings and materials looks very promising. These advancements could lead to safer and more effective treatments for heart disease and other vascular conditions.
Stent Procedure Costs and Insurance Coverage
Understanding the stent procedure costs and insurance coverage is key. The cost of a stent implantation varies. It depends on the stent type, procedure complexity, and the healthcare facility. In the U.S., the cost can be between $30,000 and $50,000 or more.
Most health insurance plans, including Medicare and Medicaid, cover stent procedures when they’re medically necessary. But, the coverage can vary. It’s important for patients to check their insurance policy and talk to their provider. This way, they can understand what they’ll pay out of pocket.
| Insurance Type | Typical Coverage for Stent Procedures |
| Private Insurance | 70-80% of the total cost, after meeting deductible |
| Medicare | 80% of the Medicare-approved amount, after meeting deductible |
| Medicaid | Varies by state, but generally covers a significant portion of the cost |
For those with high medical expenses from stent procedures, there are options. Hospitals and healthcare providers offer payment plans and discounts. Non-profit organizations and patient advocacy groups also provide financial help.
Patients should talk openly with their healthcare provider about costs. They should explore all options to manage expenses. By understanding insurance coverage and seeking help when needed, patients can make informed decisions. This way, they can reduce the financial burden of stent implantation.
The Future of Stent Technology
Medical technology is advancing fast, and stent technology is no exception. Researchers and innovators are pushing the limits to create new solutions. They aim to improve patient care and reduce complications.
New materials, coatings, and designs are being explored. These could make stents more effective and safer. This is a big step forward for treating heart diseases.
Biodegradable stents are an exciting development. They are made to dissolve in the body over time. This means no permanent implant is needed.
Biodegradable stents could change how we treat heart disease. They might reduce risks like stent thrombosis and restenosis. This could lead to better treatment options for many patients.
Stent research is also looking into advanced coatings and materials. Scientists want to find substances that help healing, reduce inflammation, and prevent scar tissue. These could lead to faster recovery times and less need for medication.
As stent technology advances, patients will have better treatment options. These options will be more personalized and less invasive. This is great news for those with cardiovascular diseases.
FAQ's
Q: Will I need to take medication because I have a stent?
A: Yes, your provider will prescribe antiplatelets to keep platelets from collecting in your stent. If they can’t gather, they can’t form a blood clot that could block your artery. You may need to take aspirin for life and another type of medicine for a year or more. Providers call this dual antiplatelet therapy because it uses two kinds of medicine.
Researchers are studying how long people need to take these medications. Providers prescribing these need to consider various factors, like your age, sex, lifestyle, other medical conditions and the specific type of stent you received.
Don’t stop taking this medicine until your provider tells you to.
Q: What is a stent, and how does it work?
A: A stent is a tiny mesh tube put in a narrowed or blocked artery. It keeps the artery open and ensures blood flow. This helps the heart muscle or other parts of the body get the blood they need.
Q: What are the different types of stents?
A: There are two main types of stents. Cardiac stents treat coronary artery disease. Vascular stents address various vascular conditions, like peripheral artery disease and carotid artery stenosis.
Q: What is the difference between bare-metal stents and drug-eluting stents?
A: Bare-metal stents are made of metal mesh without any special coating. Drug-eluting stents have a coating that releases medication to prevent scar tissue and reduce restenosis risk. Drug-eluting stents may need longer use of blood thinners than bare-metal stents.
Q: What is the stent implantation procedure like?
A: The procedure starts with angioplasty. A catheter with a balloon is guided to the narrowed or blocked artery. The balloon is then inflated to widen the artery, and a stent is placed to keep it open. The whole process is done under local anesthesia and sedation. Patients usually go home the same day or the next day.
Q: What are the possible risks and complications with stents?
A: The main risks are stent thrombosis and stent restenosis. Stent thrombosis is when a blood clot blocks the stent. Stent restenosis is when scar tissue narrows the artery again. These can be managed with medication, more procedures, or replacing the stent if needed.
Q: What lifestyle changes are recommended after stent implantation?
A: After getting a stent, patients should eat a heart-healthy diet, exercise regularly, manage stress, and quit smoking. Taking prescribed medications and attending follow-up appointments are also key to monitor stent performance and overall health.
Q: Are there any advances in stent technology?
A: Yes, stent technology has seen big advances. Biodegradable stents dissolve over time, leaving a healthy artery. New stent coatings and materials are being researched to improve performance, reduce complications, and better patient outcomes.
Q: Does insurance cover the cost of stent procedures?
A: In most cases, insurance, including Medicare and Medicaid, covers stent procedures when they’re medically necessary. But coverage can vary. It’s important to talk to your insurance provider and healthcare team to understand what’s covered and any costs you might have to pay.
One Final Note..
You may feel a little uneasy about a provider placing a manufactured part in your body. When you think of it that way, it sounds like something from a superhero comic book. But providers have been using stents for decades and the companies that make them keep improving them over time. You may feel more at ease with a stent if you learn more about it and ask your provider any questions you have.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 - K. Kerr Most recent revision February 09, 2026 07:44:04 AM
|











