- Main Page
- A1C Test
- Advance Directives
- Anxiety
- Aortic Aneurysm
- Aphrodisiacs
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation - AFib
- Back Pain
- Blood Tests
- Blood Test Tubes
- Blood Types
- BMI Calculator
- Body Mass Index - BMI
- Bone Density Scan
- Bone Scan
- BPPV
- Bronchitis
- Cancer - Lung
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- Caregiver Glossary
- Caregiver Resources - LGBTQ+
- Caregiver Resources - MO
- Caregiver Resources - USA
- Continuous Glucose Monitors
- Cholesterol
- Citalopram
- COPD
- Coronary Artery Disease
- Cough
- CPAP
- CT scan
- Cyclobenzaprine
- Degenerative Disc Disease
- Depression
- Diabetes Information
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes Facts
- Diabetes Care
- Diabetes Care Team
- Diabetes & Fruits
- Diabetes - Gestational
- Diabetes - Pre
- Diabetic Terms
- Diabetes & Vegetables
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Disability Permits
- Do Not Resuscitate
- Dupixent®
- Echocardiogram
- E-Cigarettes
- Electrocardiogram
- Electromyography
- Emphysema
- Epidural - Lumbar
- Epidural - Transforaminal
- Epsom Salt
- Facet Arthropathy
- Farxiga®
- Flu - Influenza
- Fluoroscopy
- Gabapentin
- GERD
- Glycemic Index
- Gout
- Headaches
- Healing & Energy Work
- Health Facts
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Imaging Tests
- Herbal Terms
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- HIPAA
- Home Remedies
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hyperkalemia
- Hyperlipidemia
- Hypertension
- Hypoglycemia
- Hypokalemia
- Hypotension
- Important Numbers
- Indomethacin
- Informed Consent
- Inhalers
- Insomnia
- Insulin
- Juice Fasting
- Juice Recipes
- Kidney Cysts
- Kidney Disease
- Lantus®
- Lemon Benefits
- Lime Benefits
- Liver Disease
- Lumbar Retrolisthesis
- Medicaid
- Medical Specialties
- Medicare
- Medicare - Your Rights
- Melatonin
- Men's Health
- Mental Health
- MO HealthNet
- Mounjaro®
- MRI Scan
- Myelography
- Naproxen
- Nasal Polyps
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- Otolaryngologist
- Oxycodone-Acetaminophen
- Pain Management
- Peripheral Artery Disease
- Parking Spaces
- PET/CT Scan
- PET Scan
- Potassium
- Prescription Drugs
- Prurigo Nodularis
- PVC's
- Quetiapine
- Quit Smoking
- Radiculopathy
- Red Yeast Rice
- Reiki
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- SPECT Scan
- Spinal Stenosis
- Statins
- Stents
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Support Groups
- Tardive Dyskinesia
- Testosterone
- Trazodone
- Ultrasound
- Vaccines 19 and up
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin F
- Vitamin K
- Vitamins and Minerals
- Vitamins Recommended
- Water Benefits
- X-Rays
Needed to read PDF's
MO HealthNet
What is MO HealthNet?
We may be able to help you with certain medical costs. If you are approved for help, you will have healthcare coverage through Missouri Medicaid (MO HealthNet). This healthcare coverage is different than Medicare and it can help with benefits not normally covered through that program, like nursing home care and personal care services.
Who is eligible?
Eligibility for MO HealthNet depends on your income, age, health, and individual needs. You may be eligible if you are a(n):
- Senior (age 65 and older)
- Parent or caretaker with a child (under age 19)
- Child (age birth -18)
- Woman (age 18-55) with no health insurance
- Adult (age 19-64) without disabilities
- Pregnant woman (including unborn child)
- Woman (under age 65) with breast or cervical cancer
- Person with disabilities
- Blind or visually impaired adult
How do I apply?
You can apply for healthcare coverage by completing these simple steps:
| Apply | Complete Form | Submit |
|
There are four ways you can apply for healthcare coverage: Apply through the online portal
Apply by phone at 855-373-9994 Download & print, or scan application (aplicación Español)*You must use Adobe Reader |
You must complete & submit the Supplemental Form (Forma Español) with your application if you: Are age 65 or older Are blind or disabled Get Social Security Live in a medical or nursing facility Have Medicare or VA healthcare |
You can submit your completed form(s) in one of these ways: Online: mydssupload.mo.gov
Mail:
|
When will I get coverage?
If you applied for healthcare coverage, they will let you know what might be needed to process your application. The time it takes to process your application may vary, and if they have to make an eligibility decision based on a disability, it may take longer than usual. If you do not receive anything from the Family Support Division after 45 days, you can them
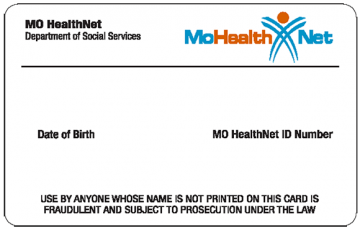
Once your application is processed, you will get a letter that let’s you know if you are eligible for healthcare coverage or not. If you are approved, you will receive a MO HealthNet Identification Card and information explaining the type of services and coverage you have. You will need to follow the instructions in this letter for your coverage to begin.
Other MO HealthNet Programs
- Spend Down: If you make too much money, you may still be able to get MO HealthNet coverage if you agree to pay, or “spend down,” a certain amount. Once you spend this amount, you will have MO HealthNet coverage for the month.
- Ticket to Work: If you are disabled and make too much money to qualify for MO HealthNet, you can still get help with your healthcare costs if you agree to take part in this program.
- Home & Community Based Services: These services may be able to help you or a loved one stay at home and out of a nursing home by providing the in-home services you need.
- MO HealthNet Nursing Home Coverage: If you live in a nursing home, they may be able to help pay for any nursing home costs you aren’t responsible for. You will be responsible for using all of your income towards costs except for a $50 monthly allowance, any health insurance premiums, and any income set aside for a spouse or other dependents.
- The Health Insurance Premium Payment (HIPP): Program helps pay for the cost of health insurance premiums for certain MO HealthNet participants.
- Supplemental Nursing Care Program: If you live in a residential care facility or assisted living facility, the Supplemental Nursing Care Program will give you a monthly allowance of $50 for personal needs and a cash payment to your facility ($156 per month for residential care or $292 per month for assisted living).
- Medicare Cost Savings Programs (QMB & SLMB): You may be able to get help paying for your Medicare premiums and certain copayments through one of the Medicare Cost Savings Programs.
- Supplemental Aid for the Blind: The Supplemental Aid for the Blind program offers a monthly cash grant and MO HealthNet coverage to help blind persons meet their basic needs.
- Blind Pension: Blind Pension offers a monthly cash grant and MO HealthNet Coverage to blind persons who do not qualify for help through Supplemental Aid to the Blind or Social Security Income benefits.
- Show-Me Healthy Babies Program: If you are pregnant and you were not approved for coverage through MO HealthNet for Pregnant Women, help may still be available through the Show-Me Healthy Babies Program.
- The Program of All-Inclusive Care for the Elderly (PACE): is administered by MO HealthNet and Medicare to provide comprehensive health care, social, recreational, and wellness services to their participants. One of the main goals of PACE is to allow older adults to live safely in their homes instead of nursing facilities.
Medicare Savings Program
Medicare is a federal healthcare coverage program for qualified adults over the age of 65, or under age 65 if they are receiving Social Security Disability benefits. The Medicare Savings Program (MSP) can help Medicare (Part A and Part B) participants pay their medical premiums.
Some participants may be eligible for:
- Help paying their Medicare deductibles and co-insurance copays
- MSP and MO HealthNet (MO HealthNet can help pay for medical costs that are not covered by Medicare)
|
Qualified Medicare Beneficiary (QMB) |
Specified Low-Income Medicare Beneficiary
(SLMB) |
Qualified Individual
Program (QI-1) |
|
|
|
Who is Eligible
Individuals may qualify for MSP, if they are:
- A U.S. Citizen (or qualified non-citizen) and Missouri resident
- Have Medicare Part A
- Meet certain income and resource requirements
How to Apply
- To apply for MSP, complete the Application for Medicare Savings Program online. You can also download and print, or scan the application. You can upload a copy of your form, or mail it to: Family Support Division | P.O. Box 2700 | Jefferson City, MO 65102, or drop it off at your local FSD Resource Center.
- If you already have MO HealthNet coverage and would like to add MSP, please visit the Change Report online, select "Request changes to your MO HealthNet coverage," enter your name, and the select "sign and submit." You can also request to add on MSP at your local FSD Resource Center.
- To apply for MSP and MO HealthNet (Missouri Medicaid), visit mydss.mo.gov/healthcare/apply or you can apply in person at your local FSD Resource Center.
Nursing Home Coverage
Nursing Home Coverage through MO HealthNet helps residents in nursing homes, or long-term care facilities, pay for room and board, as well as necessary medical and non-medical goods and services. Participants will use all of their income towards nursing home costs, except for a $50 allowance, health insurance premiums, and any income set aside for a spouse or other dependents.
Who is Eligible?
Individuals may qualify if they meet certain income requirements, and be:
- Age 65 (or older), blind, or permanently disabled
- A U.S. Citizen (or qualified non-citizen) and Missouri resident
- Approved by the Dept. of Health and Senior Services to get care from a nursing facility
- Eligible for, or currently have, MO HealthNet
There are set limits for the resources and income you can have to qualify for help through this program.
How to Apply
- If you already have coverage through MO HealthNet and you enter a nursing home/facility, you (or an authorized representative) need to let FSD know by reporting to the online Change Report, or by visiting your local FSD Resource Center.
- If you do not have MO HealthNet, you will need to apply. Visit mydss.mo.gov/healthcare/apply to get started. When you complete your application, make sure to check the box that asks if someone in the household lives in a medical facility or nursing home.
NOTE: You will know if your application was approved within 45-90 days.
Supplemental Nursing Care
The Supplemental Nursing Care Program provides monthly cash assistance to cover cost of living fees, to aged, blind, and disabled adults living in assisted living and residential care facilities. Supplemental Nursing Care (SNC) will give you a monthly allowance of $50 for personal needs, as well as a cash payment for your facility fees ($156 per month for residential care, or $292 per month for assisted living). When you apply for SNC, we will consider your monthly income from your job, Social Security, and any other sources, and will compare that amount to the monthly cost of the facility you live in. If your monthly income is less than the monthly cost of the facility, SNC could help cover the difference (up to the max amount allowed).
Who is Eligible?
Individuals may qualify if they meet certain income requirements, and are:
- Age 21 (or older)
- Live in a supported living facility (e.g. licensed residential care, assisted living, or intermediate or skilled nursing facility)
- A U.S. Citizen (or qualified non-citizen) and Missouri resident
- Have an income that is less than the monthly cost to live in the facility
- Be eligible for, or currently have, MO HealthNet
There are set limits for the resources and income you can have to qualify for help through this program.
How to Apply
- If you already have coverage through MO HealthNet and you want to add Supplemental Nursing Care, you need to complete the MO HealthNet Application Addendum and make sure to check the box for Supplemental Nursing Care. You can submit this form online, or to your local FSD Resource Center.
- If you do not have MO HealthNet, you will need to apply. Visit mydss.mo.gov/healthcare/apply to get started. When you complete your application, make sure to check the box that asks if someone in the household lives in a medical facility or nursing home.
NOTE: You will know if your application was approved within 45-90 days.
Home & Community Based Services
Home & Community Based Services provide in-home services to qualified MO HealthNet (Missouri Medicaid) participants who live at home. These services may include, home healthcare, physical or speech therapy, meal delivery or food delivery, personal care (like dressing, bathing, eating, etc.), house cleaning, and other services.
Who is eligible?
Individuals may qualify if they meet certain income requirements, and are:
- Age 63 (or older)
- A U.S. Citizen (or qualified non-citizen) and Missouri resident
- Approved by the Dept. of Health and Senior Services (DHSS) to get in-home services
- Be eligible for, or currently have, MO HealthNet
NOTE: If you are approved for Home & Community Based Services, you will not be required to spend down your MO HealthNet coverage.
How to Apply
- If you already have coverage through MO HealthNet and you want to add Home & Community Based Services, call 877-304-7939.
- If you do not have MO HealthNet, you will need to apply. Visit mydss.mo.gov/healthcare/apply to get started.
MO HealthNet Programs
MO HealthNet offers healthcare coverage through either a Managed Care health plan (also referred to as MAGI) or the Fee-For-Service Program (referred to as non-MAGI). Which program you get your services through depends on your age and eligibility. If you are not sure which program you have, log in to the FSD Benefit Portal for more information about your coverage.
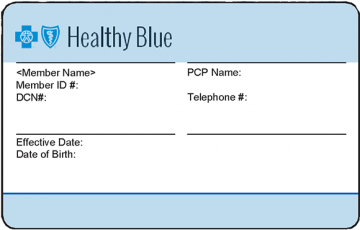
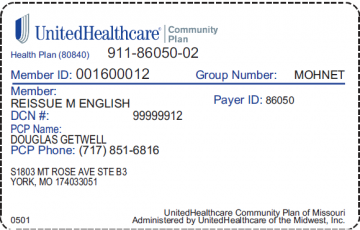
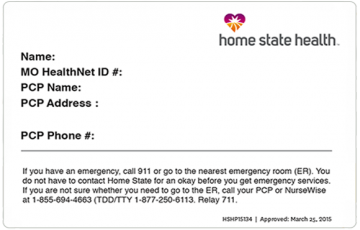
Managed Care Health Plan
You will get your MO HealthNet coverage through one of the Managed Care Health Plans: Healthy Blue, United Healthcare, or Home State Health if you are a:
- Parent or caretaker with a child under age 19
- Child age birth-18
- Woman age 18-55 with no health insurance
- Adult age 19-64 with no disabilities
- Pregnant woman (including your unborn child)
Review the Managed Care Guide for more information about your program.
Fee for Service Program
You will get your MO HealthNet coverage through the Fee-For-Service Program if you are:
- Age 65 or older
- Have a disability
- Are blind or visually impaired
- Are a woman under age 65 with breast or cervical cancer
Review the MO HealthNet Fee-For-Service Guide for more information about your program.
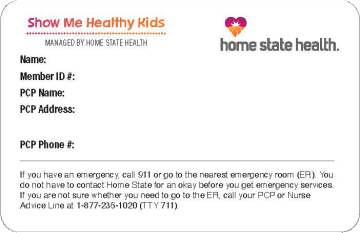
NOTE: Certain individuals will get their coverage through Show Me Healthy Kids (SMHK).
How do I contact my health plan?
If you have questions about your health plan, covered services, or your plan’s health care providers, you should reach out to your health plan directly:
If you need help with changing your health plan, call 800-348-6627. If you are in Show Me Healthy Kids, you cannot change your health plan. Translation services are available at no cost if needed. If you are deaf or hearing impaired, call Relay Missouri at 711.
How do I contact my Fee-For-Service health plan?
If you have a disability, are age 65 and over, blind or visually impaired, or have breast or cervical cancer, you most likely have MO HealthNet Fee For Service coverage.
If you have questions about your health plan or covered services, reach out to:
- Online: visit mydss.mo.gov to apply for benefits, check your status, report a change, or learn more about benefits
- Email: Ask.MHD@dss.mo.gov
- Chat Online: Visit mydss.mo.gov and select "DSS Chat" to get answers about your case or general information
- In Person: Visit your local Resource Center
- Call: Constituent Services at 800-392-2161.
Need a new card?
|
EBT Card
If your EBT card has been lost, stolen, or damaged
FSD Information Center at 855-FSD-INFO |
Healthcare Card
If you need a new MO HealthNet ID card, please call 855-FSD-INFO.
MO HealthNet |
Managed Health Plan Card
If you need a new Managed Care health plan card, please reach out to
your health plan directly.
Visit Contact
Your Health Plan for more information.
Covered Services
Refer to the chart below for what services are covered based on your type of coverage.
Work with your healthcare provider to determine if the service you need is covered.
| Service | Managed Care Members |
Fee-For-Service Participants |
| 24-hour access by phone | ✔ | |
| Adult Day Health Care | ✔ ** | |
| Ambulance | ✔ | ✔ |
| Ambulatory Surgical Center | ✔ | ✔ |
| Asthma | ✔* | ✔ |
| Behavioral Health & Substance Use Disorders (including emergency) | ✔ | ✔ ** |
| Birthing Center | ✔ | ✔ |
| Care Management | ✔ | ✔ ** |
| Chiropractic services | ✔* | ✔ |
| Complementary health & alternative therapy for chronic pain | ✔* | ✔ |
| Comprehensive Day Rehabilitation (recovery from serious head injury) | ✔* | ✔ ** |
| Diabetes education & self-management training | ✔* | ✔ |
| Diabetes Prevention Program | ✔* | ✔ |
| Dental services | ✔* | ✔ ** |
| Diabetic supplies & equipment | ✔* | ✔ ** |
| Doctor's office visits | ✔ | ✔ |
| Durable Medical Equipment | ✔* | ✔ |
| Emergency room | ✔ | ✔ |
| Family planning services | ✔ | ✔ |
| Habilitative skilled therapy services | ✔* | |
| Healthy Children & Youth (HCY) services | ✔ | ✔ |
| Hearing aids & related services | ✔* | ✔ ** |
| HIV treatment | ✔ | |
| Home Health Services | ✔* | ✔ |
| Hospice (last 6 months of life) | ✔* | ✔ |
| Hospital (overnight stay required) | ✔ | ✔ |
| Laboratory tests & x-rays | ✔ | ✔ |
| Lead poisoning | ✔ | ✔ |
| Maternity services | ✔ | ✔ |
| Nurse midwife | ✔ | ✔ |
| Nursing facility | ✔ | ✔ |
| Occupational therapy services | ✔* | ✔ ** |
| Outpatient (overnight stay not required) | ✔ | ✔ |
| Personal care | ✔ | ✔ ** |
| Pharmacy | ✔ | ✔ |
| Physical Therapy services | ✔* | ✔ ** |
| Preventative care | ✔ | ✔ |
| Podiatry (feet) | ✔* | ✔ ** |
| Sexually Transmitted Diseases | ✔ | ✔ |
| Specialist care (with provider referral) | ✔ | ✔ |
| Speech therapy services | ✔* | ✔ ** |
| Substance use treatment | ✔ | ✔ |
| Tobacco cessation counseling | ✔ | ✔ |
| Transplant related services | ✔ | ✔ |
| Transportation to medical appointments | ✔* | ✔ ** |
| Treat no transport services | ✔ | ✔ |
| Tuberculosis | ✔ | ✔ |
| Vision | ✔* | ✔ ** |
* Limited Benefit, refer to Your Guide to Managed Care or your health plan’s member handbook for more information.
** Services may be limited or not covered based on your eligibility group or age.
To find out, refer to Your Guide to Fee-For-Service or call the Participant Services Unit at 800-392-2161.
MO HealthNet Portal
You can visit the MO HealthNet Portal to get helpful information and access features to manage your benefit, including:
- View your household member information
- Opt-out of Managed Care or change health plans
- View invoices and letters
- Pay premiums and spend down
- Search for a MO HealthNet provider
- View FAQs and helpful forms
- Compare health plans
- Pay Spend Down
Your Responsibilities
Bring your healthcare card to appointments
You will get your MO HealthNet ID card in the mail, and if you have Managed Care, you will also get a health plan card. Make sure to bring ALL your cards with you to every appointment. If your ID card is lost or stolen, you will need to request a new card.
Complete an annual renewal each year
Every year, you will be required to complete an annual renewal which will check to see if you are still eligible for MO HealthNet. Typically your annual renewal will be due around the anniversary of when your MO HealthNet coverage began. For example, if you were approved for MO HealthNet in June, your renewal will be due in June each year. If you do not return your information by the deadline on the form, you may lose your coverage. Visit mydss.mo.gov/renew for more information about MO HealthNet annual renewals.
Keep your information up to date
You need to let us know if your information (address, household size, or income) has changed as soon as possible. You can report changes online any day, any time. You can also report a change by phone at 855-373-4636 or by visiting your local FSD Resource Center.
Facts About Missouri Department of Social Services
| MO HealthNet | |
| Facts | Count |
| Number of people enrolled for MO HealthNet services | 1,030,053 |
| MO HealthNet dollars spent state fiscal year 2021 | $10.04 bil |
| Estimated federal portion of MO HealthNet dollars spent | $6.53 bil |
| MO HealthNet dollars for inpatient hospital services | $534.3 mil |
| MO HealthNet dollars for physician services | $428.8 mil |
| MO HealthNet dollars for nursing home services | $1.04 bil |
| MO HealthNet dollars for pharmacy services | $1.41 bil |
| MO HealthNet dollars for managed care payments | $2.52 bil |
| Family Support | |
| Facts | Count |
| Child support collections (IV-D and non-IV-D) | $807.4 mil |
| Average monthly temporary assistance families | 8,607 |
| Total temporary assistance payments | $22.7 mil |
| Average monthly food stamp benefit recipients | 717,668 |
| Total food stamp benefits received | $1.71 bil |
| Child Protection and Permanency | |
| Facts | Count |
| Children involved in hotline reports | 73,466 |
| Children with substantiated abuse or neglect | 4,688 |
| Children with family assessments | 47,613 |
| Average monthly children in foster care | 13,924 |
| Children adopted | 1,513 |
| Total Children’s Services expenditures | $311.4 mil |
| Average monthly children receiving subsidized child care | 21,861 |
| Child care expenditures | $120.8 mil |
| Youth Services | |
| Facts | Count |
| Youths committed | 366 |
| Average monthly youths in DYS custody | 679 |
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 - K. Kerr Most recent revision February 09, 2026 07:37:06 AM
|