- Main Page
- A1C Test
- Advance Directives
- Anxiety
- Aortic Aneurysm
- Aphrodisiacs
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation - AFib
- Back Pain
- Blood Tests
- Blood Test Tubes
- Blood Types
- BMI Calculator
- Body Mass Index - BMI
- Bone Density Scan
- Bone Scan
- BPPV
- Bronchitis
- Cancer - Lung
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- Caregiver Glossary
- Caregiver Resources - LGBTQ+
- Caregiver Resources - MO
- Caregiver Resources - USA
- Continuous Glucose Monitors
- Cholesterol
- Citalopram
- COPD
- Coronary Artery Disease
- Cough
- CPAP
- CT scan
- Cyclobenzaprine
- Degenerative Disc Disease
- Depression
- Diabetes Information
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes Facts
- Diabetes Care
- Diabetes Care Team
- Diabetes & Fruits
- Diabetes - Gestational
- Diabetes - Pre
- Diabetic Terms
- Diabetes & Vegetables
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Disability Permits
- Do Not Resuscitate
- Dupixent®
- Echocardiogram
- E-Cigarettes
- Electrocardiogram
- Electromyography
- Emphysema
- Epidural - Lumbar
- Epidural - Transforaminal
- Epsom Salt
- Facet Arthropathy
- Farxiga®
- Flu - Influenza
- Fluoroscopy
- Gabapentin
- GERD
- Glycemic Index
- Gout
- Headaches
- Healing & Energy Work
- Health Facts
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Imaging Tests
- Herbal Terms
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- HIPAA
- Home Remedies
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hyperkalemia
- Hyperlipidemia
- Hypertension
- Hypoglycemia
- Hypokalemia
- Hypotension
- Important Numbers
- Indomethacin
- Informed Consent
- Inhalers
- Insomnia
- Insulin
- Juice Fasting
- Juice Recipes
- Kidney Cysts
- Kidney Disease
- Lantus®
- Lemon Benefits
- Lime Benefits
- Liver Disease
- Lumbar Retrolisthesis
- Medicaid
- Medical Specialties
- Medicare
- Medicare - Your Rights
- Melatonin
- Men's Health
- Mental Health
- MO HealthNet
- Mounjaro®
- MRI Scan
- Myelography
- Naproxen
- Nasal Polyps
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- Otolaryngologist
- Oxycodone-Acetaminophen
- Pain Management
- Peripheral Artery Disease
- Parking Spaces
- PET/CT Scan
- PET Scan
- Potassium
- Prescription Drugs
- Prurigo Nodularis
- PVC's
- Quetiapine
- Quit Smoking
- Radiculopathy
- Red Yeast Rice
- Reiki
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- SPECT Scan
- Spinal Stenosis
- Statins
- Stents
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Support Groups
- Tardive Dyskinesia
- Testosterone
- Trazodone
- Ultrasound
- Vaccines 19 and up
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin F
- Vitamin K
- Vitamins and Minerals
- Vitamins Recommended
- Water Benefits
- X-Rays
Needed to read PDF's
Sciatica
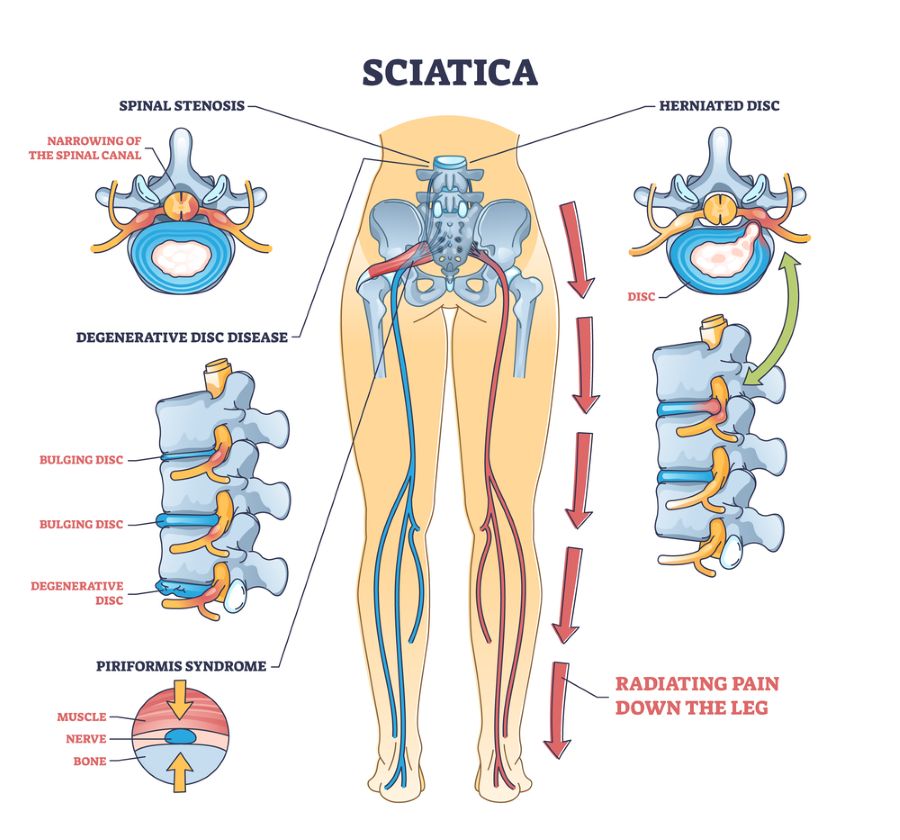
Click on picture for a full screen view
Sciatica is a common condition that causes pain, numbness, and weakness in the lower back, buttocks, and legs. It happens when the sciatic nerve gets compressed or irritated. This nerve runs from the lower back down each leg.
This can lead to severe sciatic nerve pain. The pain spreads from the lower back to one or both legs.
While sciatica can be very uncomfortable and disrupt daily life, there are many effective treatments. These include physical therapy, exercise, medications, and alternative therapies. Finding the right combination of treatments can help manage the pain and improve mobility.
In this article, we’ll explore what causes sciatica, its symptoms, and treatment options. Whether you’re dealing with sciatica now or want to prevent it, understanding this condition can help you find lasting pain relief.
What is Sciatica and How Does It Occur?
Sciatica is a common condition that causes pain, numbness, or weakness. It happens when the sciatic nerve is irritated. The sciatic nerve runs from the lower back, through the buttocks, and down each leg.
Anatomy of the Sciatic Nerve
The sciatic nerve starts from the lower spinal cord, from L4 to S3 vertebrae. It has two main branches:
| Branch | Path |
| Tibial Nerve | Runs down the back of the leg into the foot |
| Common Peroneal Nerve | Runs down the front and side of the leg into the foot |
When the sciatic nerve gets compressed or irritated, it can cause sciatica symptoms.
Types of sciatica
There are four types of sciatica. Regardless of what type you have, the effects are the same.
The types are:
1. Acute sciatica
- Caused by sudden irritation to the nerves due to pinching, compression, or a combination of both.
- Symptoms may include:
- A burning or shooting sensation throughout the lower back, buttocks, and down the leg
- Hip pain
- Difficulty sitting as symptoms get worse
- Pain can last 1-2 weeks.
2. Chronic sciatica
- Can last months or years and may occur intermittently.
- Some conditions that can worsen the pain include:
- Inflammatory conditions, such as rheumatoid arthritis
- Injuries
- Infections
- Spinal misalignment issues
- May resolve temporarily but can recur without treatment or lifestyle and activity adjustments.
3. Bilateral sciatica
- A rare type of sciatica that affects both legs.
- May be caused by multiple herniated discs or disc degeneration.
- The pain may be felt in both legs and buttocks at the same time.
- At times, pain in one leg might be more severe than pain in the other leg.
4. Alternative sciatica
- A rare type of sciatica that can cause pain in both legs alternatively.
- Can result from degenerative problems in the sacroiliac joint or sacroiliac arthritis.
Healthcare providers tend to refer to both types as just “sciatica.” The differences between them usually only matter when your healthcare provider determines how to treat it.
How common is sciatica?
Sciatica is a very common condition. About 40% of people in the U.S. experience some form of sciatica during their lifetime. It rarely happens before age 20 unless it’s injury-related.
Symptoms
Sciatica pain can be almost anywhere along the nerve pathway. It's especially likely to follow a path from the low back to the buttock and the back of a thigh and calf.
The pain can vary from a mild ache to a sharp, burning pain. Sometimes it feels like a jolt or electric shock. It can be worse when coughing or sneezing or sitting a long time. Usually, sciatica affects only one side of the body.
Some people also have numbness, tingling, or muscle weakness in the leg or foot. One part of the leg can be in pain, while another part can feel numb.
When to see a doctor
Mild sciatica usually goes away over time. Call your primary care professional if self-care measures don't ease symptoms. Also call if pain lasts longer than a week, is severe or gets worse.
Get immediate medical care for:
- Pain. Sciatica pain happens because of pressure on the affected nerve(s). Most people describe sciatica pain as burning or like an electric shock. This pain also often shoots or radiates down the leg on the affected side. Pain commonly happens with coughing, sneezing, bending or lifting your legs upward when lying on your back.
- Tingling or “pins and needles” (paresthesia). This is similar to the feeling you have when a leg falls asleep because you sat cross-legged.
- Numbness. This is when you can’t feel sensations on the skin in the affected areas of your back or leg. It happens because signals from your back or leg are having trouble reaching your brain.
- Muscle weakness. This is a more severe symptom. It means that muscle command signals are having trouble reaching their destinations in your back or legs.
- Urinary incontinence or fecal incontinence. This is a very severe symptom. It means signals that control your bladder and bowels aren’t reaching their destinations.
Causes
Sciatica can happen because of any condition that affects the sciatic nerve. It can also happen because of conditions affecting any of the five spinal nerves that bundle to form the sciatic nerve.
Conditions that can cause sciatica include:
- Herniated discs.
- Degenerative disc disease.
- Spinal stenosis.
- Foraminal stenosis.
- Piriformis syndrome.
- Spondylolisthesis.
- Osteoarthritis.
- Injuries.
- Pregnancy.
- Tumors, cysts or other growths.
- Conus medullas syndrome.
- Cauda equina syndrome.
Risk factors
Several factors can increase the likelihood of developing sciatica. These include age, lifestyle habits, and underlying health conditions. Knowing these risk factors helps individuals take preventive measures and seek timely medical attention if needed.
Age and Sciatica
As we age, our spine naturally wears down. This can lead to conditions like herniated discs or spinal stenosis. These conditions can compress the sciatic nerve. Studies show that the risk of sciatica increases with age, more so in individuals over 45 years old.
| Age Group | Relative Risk of Sciatica |
| 18-29 | Low |
| 30-44 | Moderate |
| 45-59 | High |
| 60+ | Very High |
Lifestyle Factors Contributing to Sciatica
Certain lifestyle factors can significantly increase the risk of developing sciatica. Obesity, for example, puts extra stress on the spine, potentially leading to nerve compression. A sedentary lifestyle with prolonged sitting or lack of exercise can also weaken the core muscles that support the spine, making individuals more susceptible to sciatica.
Underlying Health Conditions and Sciatica
Some underlying health conditions can contribute to the development of sciatica. Diabetes, for instance, can cause nerve damage and increase the risk of sciatica. Other conditions like osteoarthritis, spinal tumors, or infections can also compress the sciatic nerve, leading to pain and other symptoms.
By understanding these risk factors, individuals can take proactive steps to maintain a healthy spine and reduce their chances of developing sciatica. This may include maintaining a healthy weight, engaging in regular exercise, practicing good posture, and managing underlying health conditions effectively.
Diagnosis
A healthcare provider can diagnose sciatica using a combination of methods. They’ll review your medical history and ask about your symptoms. They’ll also do a physical examination. That exam will include:
- Walking. Sciatica often causes visible changes in how you walk. Your provider will watch for those changes as part of diagnosing sciatica.
- Straight leg raise test. This involves having you lie on an exam table with your legs straight out. They’ll slowly raise your legs one at a time toward the ceiling and ask when you start to feel pain or other symptoms. These can help pinpoint the cause of sciatica and how to manage it.
- Other flexibility and strength checks. These can help your provider determine if any other factors are causing or contributing to your sciatica.
Tests
People with severe pain or pain that doesn't improve within a few weeks may need:
- X-ray. A spine X-ray is an imaging test that uses electromagnetic waves to take detailed pictures of the bones in your neck and back. You might need spinal X-rays if you were born with structural spine issues or if you have pain from trauma or conditions like arthritis or osteoporosis.
- MRI. An MRI (magnetic resonance imaging) scan is a test that creates clear images of the structures inside your body using a large magnet, radio waves and a computer. Healthcare providers use MRIs to evaluate, diagnose and monitor several different medical conditions.
- CT Scan. A CT (computed tomography) scan is an imaging test that helps healthcare providers detect diseases and injuries. It uses a series of X-rays and a computer to create detailed images of your bones and soft tissues. A CT scan is painless and noninvasive. You might go to a hospital or imaging center for your CT scan.
- Nerve conduction velocity studies. A nerve conduction study is a test that can help diagnose issues with your peripheral nerves, such as peripheral neuropathy and nerve compression syndromes. Healthcare providers often use this test alongside an EMG (electromyography) test.
- Electromyography (EMG). Neurologists use electromyography (EMG) to help diagnose injuries and conditions that affect your muscles and the nerves that control them, such as carpal tunnel syndrome and muscular dystrophy. They often use this test alongside a nerve conduction study.
- Myelogram. A myelogram is an imaging test that uses a contrast material and X-rays or computed tomography (CT) scans to get detailed pictures of your spine. Healthcare providers might recommend a myelogram if you have chronic back pain.
Treatment
Cold
You can use ice packs or even use a package of frozen vegetables.
Wrap the ice pack or frozen vegetables in a towel and apply it to the affected area for short intervals several times per day, during the first few days of symptoms. This can help to reduce swelling and ease pain.
Heat
You can also use hot packs or a heating pad.
It’s recommended that you use ice during the first couple of days to reduce swelling. After 2 or 3 days, switch to heat. Heat can help relax muscles in the back, which can spasm when an injury occurs. If you continue to have pain, try alternating between ice and heat therapy.
Stretching
Gently stretching your lower back can also be helpful. To learn how to stretch properly, get one-on-one physical therapy or even yoga instruction from a physical therapist or instructor trained to deal with your injury, if it’s available.
You may also look for free videos online to help you find the proper stretches. Make sure to consult with a medical professional first before starting a stretching routine.
Over-the-counter medication
Over-the-counter medications, such as aspirin and ibuprofen, can also help with pain, inflammation, and swelling. Be careful about using aspirin excessively, since it could cause complications, such as stomach bleeding and ulcers.
Regular exercise
The more you stay active, the more endorphins your body releases. Endorphins are pain relievers made by your body. Stick to low impact activities at first, such as swimming and stationary bicycling.
As your pain decreases and your endurance improves, create an exercise regimen that includes aerobics, core stability, and strength training. A regimen with these components can decrease your risk of future back problems. Always talk with a medical professional before starting a new exercise routine to make sure it is safe for you.
For pain that doesn't improve with self-care measures, some of the following treatments might help.
Prescription Medications
The types of medicines that might be used to treat sciatica pain include:
- Anti-inflammatories.
- Corticosteroids.
- Antidepressants.
- Anti-seizure medications.
- Opioids.
Physical therapy
Once the pain improves, a healthcare professional can design a program to help prevent future injuries. This typically includes exercises to correct posture, strengthen the core and improve range of motion. The goal of physical therapy is to find exercise movements that decrease sciatica by reducing pressure on the nerve. Options include stretching exercises or low-impact activities like walking, swimming or water aerobics.
Steroid injections
Injections like corticosteroids may provide short-term relief (typically up to three months). These usually involve local anesthesia, so there’s less discomfort. Your healthcare provider can tell you more about this process.
Surgery
Surgery may be the best option when sciatica is more severe. Usually, healthcare providers don’t recommend surgery unless you have symptoms that indicate nerve damage is happening or imminent. They may also recommend surgery if you have severe pain that prevents you from working or going about your usual routine, or if your symptoms don’t improve after six to eight weeks of conservative treatment.
Surgery options to relieve sciatica include:
- discectomy. This is a surgery that removes fragments or small sections of a herniated disc that are pressing on a nerve.
- Laminectomy. Each vertebra has a rear section called the lamina (it’s on the side of the vertebra just underneath the skin of your back). A laminectomy involves removing a section of the lamina that’s pressing on spinal nerves.
Natural treatment
Complementary medicine is growing in popularity. There are a number of remedies that could potentially help with sciatica pain. These include the following:
- In acupuncture, a practitioner inserts sterilized needles into specific points in your body, which may help improve your back pain symptoms.
- Chiropractors can make spinal adjustments or manipulations to restore spinal movement and decrease pain. Spinal manipulation appears to work and to be as safe as standard treatments for low back pain
- A massage therapist can apply motion, pressure, tension, or vibration to your body to help relieve pressure and sciatic pain symptoms.
- Ask your doctor for a referral to a specialist who performs biofeedback therapy, a mind-body technique shown to improve back pain and chronic pain. This technique uses electrical sensors to help you understand how your body responds to stress and pain.
- Committing to a mindfulness meditation practice may help reduce your pain and increase your quality of life.
Lifestyle Modifications for Sciatica Prevention and Management
Making simple lifestyle changes can help prevent and manage sciatica pain. Focus on ergonomics, exercise, and stretching. These steps can lower your risk of sciatica and ease symptoms.
Ergonomic Adjustments for Sciatica Prevention
Good posture and ergonomics are key for preventing sciatica. When sitting, keep your back straight and supported. Your feet should be flat on the floor. Adjust your workspace to support good posture:
| Workstation Component | Ergonomic Adjustment |
| Chair | Ensure the chair supports the natural curve of your lower back |
| Monitor | Position the top of the screen at eye level to avoid neck strain |
| Keyboard and Mouse | Keep them at a height that allows your elbows to rest at a 90-degree angle |
When lifting heavy objects, bend at the knees and keep your back straight. This avoids putting too much strain on your lower back and sciatic nerve.
Exercise and Stretching Routines for Sciatica Management
Regular exercise and stretching can help manage sciatica symptoms. They strengthen your core and improve flexibility. Some good exercises include:
- Pelvic tilts: Lie on your back with your knees bent and feet flat on the floor. Tilt your pelvis upward, holding for 5 seconds, then relax. Repeat 10 times.
- Knee-to-chest stretches: Lie on your back and bring one knee up to your chest, holding it with both hands. Hold for 20-30 seconds, then release and repeat with the other leg.
- Gentle yoga poses: Poses like Cat-Cow, Child’s Pose, and Pigeon Pose can help stretch and strengthen the muscles that support your lower back and sciatic nerve.
Always listen to your body and avoid any exercises or stretches that cause pain. Talk to a physical therapist or healthcare provider to create an exercise plan that fits your needs.
Preparing for your appointment
Not everyone who has sciatica needs medical care. If your symptoms are serious or last for more than a month, make an appointment with your healthcare professional.
What you can do
- Write down your symptoms and when they began.
- List key medical information, including other conditions you have and the names and doses of medications, Vitamins or supplements you take.
- Note recent accidents or injuries that might have damaged your back.
- Take a family member or friend along, if possible. Someone who accompanies you can help you remember the information you get.
- Write down questions to ask your healthcare professional.
For radiating low back pain, some basic questions to ask include:
- What's the most likely cause of my back pain?
- Are there other possible causes?
- What tests do I need?
- What treatment do you recommend?
- Should I have surgery? Why or why not?
- Are there restrictions I need to follow?
- What self-care measures should I take?
- What can I do to keep my symptoms from coming back?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- Do you have numbness or weakness in your legs?
- Do some body positions or activities make your pain better or worse?
- How much does your pain limit your activities?
- Do you do heavy physical work?
- Do you exercise regularly? If yes, with what types of activities?
- What treatments or self-care measures have you tried? Has anything helped?
What is the prognosis for sciatica?
Depending on the precise cause of sciatica and the duration of symptoms, the outlook for recovery from sciatica ranges from excellent to having long-term chronic symptoms.
The duration of sciatica is critically dependent on its cause. A herniated disc, back sprain, shingles, and degenerative lumbar spine can all cause temporary forms of sciatica, lasting from days to weeks. Each can also cause chronic sciatica.
Sometimes degeneration of the lumbar spine and discs can cause chronic sciatica that persists unless surgical intervention is performed.
Pain Management Strategies
Living with chronic sciatica can be tough, but there are ways to manage the pain. Mindfulness, relaxation, and support groups can help. These strategies can improve your life and outlook.
Mindfulness and Relaxation Techniques for Sciatica Pain
Mindfulness and relaxation are great for managing sciatica pain. They help you stay present, reduce stress, and feel calm. Here are some effective techniques:
| Technique | Benefits |
| Deep breathing exercises | Reduces tension and promotes relaxation |
| Progressive muscle relaxation | Helps release muscle tension and eases pain |
| Guided imagery | Focuses the mind on positive, calming images to distract from pain |
| Meditation | Cultivates mindfulness and reduces stress, which can exacerbate pain |
Adding these techniques to your daily life can help manage sciatica pain. It can also improve your overall well-being.
Support Groups and Counseling for Chronic Sciatica
Dealing with chronic sciatica can be tough emotionally. Having a strong support system is key. Joining a support group can offer a sense of community and understanding.
Support groups let you share experiences and learn from others. You can also find valuable coping strategies. Seeking counseling or therapy can also help with the emotional side of chronic sciatica. A mental health professional can teach you coping mechanisms and help with depression or anxiety.
Remember, you don’t have to face chronic sciatica alone. Mindfulness, relaxation, support groups, and counseling can help manage pain. They can also improve your overall quality of life.
Sciatica and Related Conditions
Sciatica often happens with other spine and nerve issues. Knowing how sciatica connects with these conditions helps get a better diagnosis and treatment plan.
Lumbar spinal stenosis is a common issue. It’s when the spinal canal in the lower back narrows. This can press on the sciatic nerve, causing pain. It’s often due to aging, like thickened ligaments or bone spurs.
Another issue is degenerative disc disease. It happens when the discs between the spine’s vertebrae wear out. This can make the discs bulge or herniate, pressing on nerves like the sciatic. This pressure leads to pain and other symptoms.
Spondylolisthesis is when a vertebra slips forward over another. This can narrow the spinal canal, putting pressure on nerves. It can be caused by aging, injury, or birth defects.
Healthcare professionals look at these conditions when treating sciatica. By addressing the root cause, like lumbar spinal stenosis or degenerative disc disease, people can find relief. This improves their quality of life.
When to Seek Medical Attention for Sciatica
Sciatica can usually be treated without needing a doctor. But, there are times when you should see a healthcare professional right away. If your pain doesn’t get better or gets worse, you should get help. This is true if you also have trouble controlling your bowel or bladder.
This could mean you have cauda equina syndrome, a serious issue that needs quick medical help.
Also, if your leg gets weaker over time, you need to see a doctor fast. This could mean your nerves are being compressed or damaged. If you have sudden, sharp pain in your back or leg, don’t ignore it. Look for numbness or tingling too. A doctor can check if there’s something serious going on.
Sciatica can be tough, but most people get better with the right care. If you notice any warning signs, don’t wait. Get medical help to ease your pain and avoid bigger problems.
Additional Common Questions
Q: What is sciatica, and what are its main symptoms?
A: Sciatica is a condition that causes pain, numbness, tingling, or weakness. It affects the sciatic nerve, which runs from the lower back to the legs. Symptoms include sharp pain in the lower back, hip, or leg, numbness or tingling in the leg or foot, and muscle weakness in the affected leg.
Q: What are the common causes of sciatica?
A: Sciatica can be caused by herniated or bulging discs, spinal stenosis, and piriformis syndrome. These conditions can irritate the sciatic nerve, leading to pain and other symptoms.
Q: What are the risk factors for developing sciatica?
A: Risk factors include age, obesity, and a sedentary lifestyle. Jobs that involve heavy lifting or prolonged sitting also increase the risk. Staying active and maintaining good posture can help prevent sciatica.
Q: How is sciatica diagnosed, and what tests are involved?
A: Diagnosing sciatica involves a physical exam and patient history. Imaging tests like MRI or CT scans may be used to see the spine and identify issues.
Q: What are the conservative treatment options for managing sciatica pain?
A: Treatment options include physical therapy, pain relief medications, and alternative therapies like acupuncture. Using heat or cold packs and practicing good posture can also help.
Q: When is surgery considered for sciatica, and what are the common procedures?
A: Surgery is considered for severe cases that don’t respond to other treatments. Procedures include laminectomy, discectomy, and spinal fusion. The decision to have surgery should be made with a healthcare provider.
Q: What lifestyle modifications can help prevent or manage sciatica?
A: Maintaining a healthy weight, exercising regularly, and practicing good posture can help. Using ergonomic furniture and staying hydrated also supports spinal health.
Q: How can individuals cope with chronic sciatica and manage pain long-term?
A: Coping with chronic sciatica involves pain management strategies like mindfulness and low-impact exercises. Working with a healthcare provider to develop a treatment plan is also important.
Can sciatica occur down both legs?
Sciatica usually affects only one leg at a time. However, sciatica can occur in both legs in rare cases.
Does sciatica occur suddenly, or does it take time to develop?
Sciatica can come on suddenly or gradually. It depends on the cause. A disc herniation or injury can cause sudden pain. Arthritis in your spine or other degenerative conditions develop slowly over time.
Can weight gain during pregnancy cause sciatica?
Sciatica is common in pregnancy but isn’t usually related to pregnancy weight changes. Two main factors better explain why it’s more likely to happen during pregnancy.
The first explanation has to do with pregnancy-related hormones. Those hormones can cause a loosening of ligaments and connective tissue in your spine. That loosening makes your spine more flexible, which can cause disc slippage, pinched nerves and sciatica.
The weight and position of the fetus can also press on the nerve.
The good news is there are ways to ease sciatic pain during pregnancy, and the pain should go away after birth. Physical therapy and massage therapy, warm showers, heat, medications and other measures can help. Practicing good posture techniques during pregnancy can also help.
How can I tell if pain in my hip is a hip issue or sciatica?
Hip problems, such as arthritis in your hip, usually cause pain in your groin, or pain when you put weight on your leg or move it around.
If your pain starts in your back and moves or radiates toward your hip or down your leg, or you have numbness, tingling or weakness, sciatica is the most likely cause.
Sciatica vs. radiculopathy — what’s the difference?
Radiculopathy is a broader term that describes the symptoms caused by a pinched nerve in your spine. Sciatica is the most common type of radiculopathy.
Should I rest if I have sciatica?
Rest is helpful during the first two days you have sciatica. But total rest isn’t likely to help, and physical inactivity can make your pain worse and slow healing. The goal is to find a balance so you’re active enough to stay flexible and maintain strength but not make sciatica worse or injure yourself. A healthcare provider can guide you on how to find this balance and help you recover.
Can sciatica cause my leg and/or ankle to swell?
Sciatica from a herniated disc, spinal stenosis or bone spurs can cause inflammation or swelling in the affected leg. Piriformis syndrome complications can also cause leg swelling.
One Final Note..
Sciatica is a painful sensation that happens when the sciatic nerve is irritated. If you have sciatica, you may feel moderate to severe pain in addition to weakness or numbness in your back, buttocks, and legs. Using hot and cold compresses, stretching, taking over-the-counter pain medications, and regularly exercising may help you manage your pain.
You can also talk with a doctor about physical therapy, prescription medication, steroid medications, and surgery for severe situations. Using complementary treatments alongside medical treatments may provide further relief.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 - K. Kerr Most recent revision February 09, 2026 07:44:04 AM
|











