- Main Page
- A1C Test
- Advance Directives
- Anxiety
- Aortic Aneurysm
- Aphrodisiacs
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation - AFib
- Back Pain
- Blood Tests
- Blood Test Tubes
- Blood Types
- BMI Calculator
- Body Mass Index - BMI
- Bone Density Scan
- Bone Scan
- BPPV
- Bronchitis
- Cancer - Lung
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- Caregiver Glossary
- Caregiver Resources - LGBTQ+
- Caregiver Resources - MO
- Caregiver Resources - USA
- Continuous Glucose Monitors
- Cholesterol
- Citalopram
- COPD
- Coronary Artery Disease
- Cough
- CPAP
- CT scan
- Cyclobenzaprine
- Degenerative Disc Disease
- Depression
- Diabetes Information
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes Facts
- Diabetes Care
- Diabetes Care Team
- Diabetes & Fruits
- Diabetes - Gestational
- Diabetes - Pre
- Diabetic Terms
- Diabetes & Vegetables
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Disability Permits
- Do Not Resuscitate
- Dupixent®
- Echocardiogram
- E-Cigarettes
- Electrocardiogram
- Electromyography
- Emphysema
- Epidural - Lumbar
- Epidural - Transforaminal
- Epsom Salt
- Facet Arthropathy
- Farxiga®
- Flu - Influenza
- Fluoroscopy
- Gabapentin
- GERD
- Glycemic Index
- Gout
- Headaches
- Healing & Energy Work
- Health Facts
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Imaging Tests
- Herbal Terms
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- HIPAA
- Home Remedies
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hyperkalemia
- Hyperlipidemia
- Hypertension
- Hypoglycemia
- Hypokalemia
- Hypotension
- Important Numbers
- Indomethacin
- Informed Consent
- Inhalers
- Insomnia
- Insulin
- Juice Fasting
- Juice Recipes
- Kidney Cysts
- Kidney Disease
- Lantus®
- Lemon Benefits
- Lime Benefits
- Liver Disease
- Lumbar Retrolisthesis
- Medicaid
- Medical Specialties
- Medicare
- Medicare - Your Rights
- Melatonin
- Men's Health
- Mental Health
- MO HealthNet
- Mounjaro®
- MRI Scan
- Myelography
- Naproxen
- Nasal Polyps
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- Otolaryngologist
- Oxycodone-Acetaminophen
- Pain Management
- Peripheral Artery Disease
- Parking Spaces
- PET/CT Scan
- PET Scan
- Potassium
- Prescription Drugs
- Prurigo Nodularis
- PVC's
- Quetiapine
- Quit Smoking
- Radiculopathy
- Red Yeast Rice
- Reiki
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- SPECT Scan
- Spinal Stenosis
- Statins
- Stents
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Support Groups
- Tardive Dyskinesia
- Testosterone
- Trazodone
- Ultrasound
- Vaccines 19 and up
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin F
- Vitamin K
- Vitamins and Minerals
- Vitamins Recommended
- Water Benefits
- X-Rays
Needed to read PDF's
Heart Disease
Key points
- Coronary artery disease is the most common type of heart disease.
- There are many other conditions that affect the heart.
- The term "heart disease" refers to several types of heart conditions.
- Know your risk for heart disease so you can prevent it.
- High blood pressure, high blood cholesterol, and smoking are key risk factors.
- About 1 in 5 people in the United States died from heart disease in 2022.
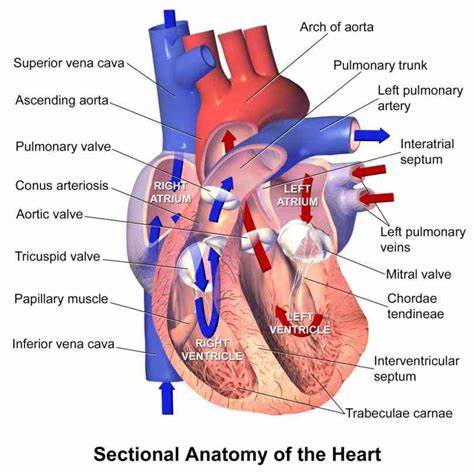
What is heart disease?
Heart disease is a variety of issues that can affect your heart. When people think about heart disease, they often think of the most common type — coronary artery disease (CAD) and the heart attacks it can cause. But you can have trouble with different parts of your heart, like your heart muscle, valves or electrical system.
When your heart isn’t working well, it has trouble sending enough blood, oxygen and nutrients to your body. In a way, your heart delivers the fuel that keeps your body’s systems running. If there’s a problem with delivering that fuel, it affects everything your body’s systems do.
Lifestyle changes and medications can keep your heart healthy and lower your chances of getting heart disease.
What causes heart disease?
The most common type of heart disease is coronary artery disease (CAD), and the leading cause of CAD is atherosclerosis, the buildup of cholesterol plaque inside the coronary arteries. Too much plaque limits blood flow through the arteries that supply blood to the heart. Restricted blood flow can cause chest pain or pressure (known as angina) and requires immediate medical attention. When plaque ruptures, it can form a blood clot that stops blood flow and triggers a heart attack.
The risk factors for atherosclerosis (and thus CAD) include:
- high total blood cholesterol level
- high level of LDL (bad) cholesterol
- high levels of triglycerides
- high levels of lipoprotein(a)
- high blood pressure (hypertension)
- diabetes
- family history of heart disease
- smoking
- obesity
- physical inactivityiInflammation
Symptoms
A variety of symptoms and signs may indicate heart disease. If you experience any of the following for no apparent reason, immediately report them to your doctor.
Fatigue. Fatigue can be caused by many illnesses and medicines. But constant, new fatigue can sometimes signal two kinds of heart disease: heart failure and coronary artery disease.
Unexplained aches or pains. Blockage of blood to the heart muscle can cause pain or pressure in the chest, shoulders, arms, back, jaw, or abdomen, primarily when pain in these locations occurs with exercise and disappears with rest.
Shortness of breath. Unexplained shortness of breath that occurs with small amounts of activity.
Swollen legs, feet, or ankles. The kind of swelling that leaves an indentation if you press your finger into it could be a sign of heart failure.
Heart palpitations. Palpitation refers to a heartbeat that feels irregular or rapid. Most palpitations may be caused by anxiety, caffeine intake, or dehydration. But sometimes they indicate a heart problem.
Sometimes heart disease may be "silent" and not diagnosed until a person experiences signs or symptoms of a heart attack, heart failure, or an arrhythmia. When these events happen, symptoms may include:
- Heart attack: Chest pain or discomfort, upper back or neck pain, heartburn, nausea or vomiting, extreme fatigue, dizziness, and shortness of breath.
- Arrhythmia: Fluttering feelings in the chest (palpitations).
- Heart failure: Shortness of breath, fatigue, or swelling of the feet, ankles, legs, abdomen, or neck veins.
Conditions related to heart disease
Coronary artery disease, also called Coronary Heart Disease or ischemic heart disease, is the most common type of heart disease, but there are many other conditions that affect the heart.
- Acute coronary syndrome is a term that includes heart attack and unstable angina.
- Angina, a symptom of coronary artery disease, is chest pain or discomfort that happens when the heart muscle is not getting enough blood. Angina may feel like pressure or a squeezing pain in the chest. The pain also may occur in the shoulders, arms, neck, jaw, or back. It may feel like indigestion.
- There are two forms of angina—stable or unstable:
- Stable angina happens during physical activity or under mental or emotional stress.
- Unstable angina is chest pain that occurs even while at rest, without apparent reason. This type of angina is a medical emergency.
- Aortic aneurysm and dissection are conditions that can affect the aorta, the major artery that carries blood from the heart to the body. An aneurysm is an enlargement in the aorta that can rupture or burst. A dissection is a tear in the aorta, which is a medical emergency. For more information, see the aortic aneurysm information page.
- Arrhythmias are irregular or unusually fast or slow heartbeats. Arrhythmias can be serious. One example is called ventricular fibrillation. This type of arrhythmia causes an abnormal heart rhythm that leads to death unless treated right away with an electrical shock to the heart (called defibrillation). Other arrhythmias are less severe but can develop into more serious conditions, such as atrial fibrillation, which can cause a stroke. see the arrhythmias information page
- Atherosclerosis happens when plaque builds up in the arteries that supply blood to the heart (called coronary arteries). Plaque is made up of cholesterol deposits. Plaque buildup causes arteries to narrow over time.
- Atrial fibrillation is a type of arrhythmia that can cause rapid, irregular beating of the heart's upper chambers. Blood may pool and clot inside the heart, increasing the risk for heart attack and stroke. For more information, see the atrial fibrillation information page.
- Cardiomyopathy happens when the heart muscle becomes enlarged or stiff. This can lead to inadequate heart pumping (or weak heart pump) or other problems. Cardiomyopathy has many causes, including family history of the disease, prior heart attacks, uncontrolled high blood pressure, and viral or bacterial infections.
- Congenital heart defects are problems with the heart that are present at birth. They are the most common type of major birth defect. Examples include abnormal heart valves or holes in the heart's walls that divide the heart's chambers. Congenital heart defects range from minor to severe.
- Heart failure is often called congestive heart failure because of fluid buildup in the lungs, liver, legs, and feet. Heart failure is a serious condition that occurs when the heart can't pump enough blood to meet the body's needs. It does not mean that the heart has stopped but that muscle is too weak to pump enough blood. Most of heart failure cases are chronic, or long-term heart failures. The only cure for heart failure is a heart transplant. However, heart failure can be managed with medications or medical procedures. For more information, see the heart failure information page.
- Marfan syndrome. Marfan syndrome is a genetic condition that affects connective tissue, which provides support for the body and organs. It can damage the blood vessels, heart, eyes, skin, lungs, and the bones of the hips, spine, feet, and rib cage.
- Mental health disorders can be short- or long-term and can interfere with a person's mood, behavior, thinking, and ability to relate to others. Various studies have shown the impact of trauma, depression, anxiety, and stress on the body, including stress on the heart. see the mental health information page.
- Peripheral arterial disease (PAD) happens when the arteries that supply blood to the arms and legs (the periphery) become narrow or stiff. PAD usually results from atherosclerosis, the buildup of plaque and narrowing of the arteries. With this condition, blood flow and oxygen to the arm and leg muscles are low or even fully blocked. Signs and symptoms include leg, calf, buttock, hip, or thigh pain, and numbness in the feet. see the Peripheral arterial disease information page
- Pulmonary hypertension happens when the pressure in the arteries leading from the heart to the lungs is too high. There are many conditions that lead to pulmonary hypertension, including connective tissue disease, liver disease, emphysema, and chronic blood clots in the lungs. Symptoms of pulmonary hypertension include shortness of breath and fatigue.
- Rheumatic heart disease is a complication of rheumatic fever. Rheumatic fever can develop after a sore throat caused by streptococcal bacteria. The infection can cause damage to the heart valves.
- Valvular heart disease. Healthy heart valves can fully open and close during a heartbeat, but diseased valves cannot. If the heart valves are diseased, the heart can't effectively pump blood throughout the body and must work harder to pump. This can lead to heart failure, sudden cardiac arrest (when the heart stops beating), heart palpitations (rapid, fluttering, or pounding), shortness of breath, or swelling in your legs and feet.
Diagnosis
Heart diseases are the number one killer in the United States. They are also a major cause of disability. If you do have heart disease, it is important to find it early, when it is easier to treat. Blood tests and heart health tests can help find heart diseases or identify problems that can lead to heart diseases. There are several different types of heart health tests. Your health care provider will decide which test or tests you need, based on your symptoms (if any), risk factors, and medical history.
Tests
Many different tests are used to diagnose heart disease.
- Blood tests. Certain heart proteins slowly leak into the blood after heart damage from a heart attack. Blood tests can be done to check for these proteins. A high-sensitivity C-reactive protein (CRP) test checks for a protein linked to inflammation of the arteries. Other blood tests may be done to check cholesterol and blood sugar levels.
- Chest X-ray. A chest x-ray creates pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels. It can reveal signs of heart failure, as well as lung disorders and other causes of symptoms not related to heart disease.
- Electrocardiogram (ECG or EKG). An electrocardiogram, also called an ECG or EKG, is a painless test that detects and records your heart's electrical activity. It shows how fast your heart is beating and whether its rhythm is steady or irregular. An EKG may be part of a routine exam to screen for heart disease. Or you may get it to detect and study heart problems such as heart attacks, arrhythmia, and heart failure. For the test, you lie still on a table and a nurse or technician attaches electrodes (patches that have sensors) to the skin on your chest, arms, and legs. Wires connect the electrodes to a machine that records your heart's electrical activity.
- Holter monitoring. A Holter monitor is a portable ECG device that's worn for a day or more to record the heart's activity during daily activities. This test can detect irregular heartbeats that aren't found during a regular ECG exam.
- Echocardiogram. Echocardiography, or echo, is a painless test that uses sound waves to create moving pictures of your heart. The pictures show the size and shape of your heart. They also show how well your heart's chambers and valves are working. Providers use an echo to diagnose many different heart problems, and to check how severe they are. There are several different types of echocardiography. For transthoracic echocardiography (the most common type), a technician applies gel to your chest. The gel helps sound waves reach your heart. The technician moves a transducer (wand-like device) across your chest. The transducer connects to a computer. It transmits ultrasound waves into your chest, and the waves bounce (echo) back. The computer converts the echoes into pictures of your heart.
- Exercise tests or stress tests. Stress testing looks at how your heart works during physical stress. It can help to diagnose coronary artery disease, and to check how severe it is. It can also check for other problems, including heart valve disease and heart failure. For the test, you exercise (or are given medicine if you are unable to exercise) to make your heart work hard and beat fast. While this is happening, you get an EKG and blood pressure monitoring. Before or after the test, you might also have an echocardiogram, or other imaging tests such as a nuclear scan. For the nuclear scan, you get an injection of a tracer (a radioactive substance), which travels to your heart. Special cameras detect the energy from the tracer to craeate pictures of your heart. You have pictures taken after you exercise, and then after you rest.
- Cardiac catheterization. Cardiac catheterization is a medical procedure used to diagnose and treat some heart conditions. For the procedure, your provider puts a catheter (a long, thin, flexible tube) into a blood vessel in your arm, groin, or neck, and threads it to your heart. The provider can use the catheter to:
- Do a coronary angiography. This involves putting a special type of dye in the catheter, so the dye can flow through your bloodstream to your heart. Then your provider takes x-rays of your heart. The dye allows your provider to see your coronary arteries on the x-ray, and to check for coronary artery disease (CAD). CAD is caused by plaque buildup in the arteries.
- Take samples of your blood and heart muscle.
- Examine your heart valves.
- Do procedures such as angioplasty or minor heart surgeries to repair congenital heart defects or replace heart valves.
- Heart CT scan, also called cardiac CT scan. A cardiac CT (computed tomography) scan is a painless imaging test that uses x-rays to take detailed pictures of your heart and its blood vessels. Computers can combine these pictures to create a three-dimensional (3D) model of your whole heart. This test can help providers detect or evaluate various heart problems, including:
- Coronary artery disease
- Calcium buildup in the coronary arteries
- Congenital heart defects
- Problems with the aorta (the main artery that carries blood away from the heart)
- Problems with heart function and valves
- Pericardial diseases
Before you have the test, you get an injection of contrast dye. The dye highlights your heart and blood vessels in the pictures. The CT scanner is a large, tunnel-like machine. You lie still on a table that slides you into the scanner, and the scanner takes the pictures.
- Heart magnetic resonance imaging (MRI) scan. Cardiac MRI (magnetic resonance imaging) is a painless imaging test that uses radio waves, magnets, and a computer to create detailed pictures of your heart. It can help your provider figure out whether you have heart disease, and if so, how severe it is. A cardiac MRI can also help your provider decide the best way to treat heart problems such as:
- Congenital heart defects
- Coronary artery disease
- Heart valve problems
- Pericarditis
- Cardiac tumors
- Damage from a heart attack
The MRI is a large, tunnel-like machine. You lie still on a table that slides you into the MRI machine. The machine makes loud noises as it takes pictures of your heart. Sometimes before the test, you might get an injection of contrast dye. The dye highlights your heart and blood vessels in the pictures.
- Coronary Angiography. Coronary angiography (angiogram) is a procedure that uses contrast dye and x-ray pictures to look at the insides of your arteries. It can show whether plaque is blocking your arteries and how severe the blockage is. Providers use this procedure to diagnose heart diseases after chest pain, sudden cardiac arrest (SCA), or abnormal results from other heart tests such as an EKG or a stress test. You usually have a cardiac catheterization to inject the dye into your coronary arteries. Then the provider will take special x-rays while the dye is flowing through your coronary arteries. The dye lets your provider study the flow of blood through your heart and blood vessels.
Treatment and recovery
Heart disease treatment depends on the cause and type of heart damage. Treatment for heart disease may include:
- Lifestyle changes such as eating a diet low in salt and saturated fat, getting more exercise, and not smoking.
- Medicines.
- A heart procedure.
- Heart surgery.
Medications
Anticoagulants
Some commonly prescribed include:
- Apixaban
- Dabigatran
- Edoxaban
- Heparin
- Rivaroxaban
- Warfarin
What the medication does
Sometimes called blood thinners, although they do not actually thin the blood. Decreases the clotting ability of the blood. They are used to treat certain blood vessel, heart and lung conditions.
Reason for medication
- Helps to prevent blood clots from forming in the blood vessels.
- May prevent the clots from becoming larger and causing more serious problems.
- Often prescribed to prevent first or recurrent stroke or heart attack.
Antiplatelet agents and dual antiplatelet therapy (DAPT)
Some commonly prescribed include:
- Aspirin
- Clopidogrel
- Dipyridamole
- Prasugrel
- Ticagrelor
What the medication does
Keeps blood clots from forming by preventing blood platelets from sticking together.
Reason for medication
- Helps stop clotting in people who have had a heart attack, unstable angina, ischemic strokes, TIA (transient ischemic attacks) and other forms of cardiovascular disease.
- Can be used preventively when plaque buildup is evident but there is not yet a major blockage in the artery.
- Can stop clots from forming inside stents or after coronary bypass graft surgery (CABG).
- Certain people will be prescribed aspirin and another antiplatelet drug. This is known as dual antiplatelet therapy (DAPT).
Dual antiplatelet therapy
Some people are treated with two types of antiplatelet agents at the same time to prevent blood clotting. It can be used for people who have:
- Heart attacks
- Stents placed in their coronary arteries
- Coronary artery bypass graft surgery (CABG)
- Stroke and transient ischemic attacks
- Angioplasty
One antiplatelet agent is aspirin. Many people with coronary artery disease are treated with aspirin for the rest of their lives. A second antiplatelet agent, called a P2Y12 inhibitor, is usually prescribed for months or years in addition to the aspirin therapy.
The type of medication and length of treatment will vary based on your condition and other risk factors. Talk to your health care professional about the risks and benefits of DAPT.
- If you had a heart attack, it is recommended that you be on DAPT for at least a year. If you don’t have a high bleeding risk, taking it longer may lower your risk of a future heart attack.
- If you received a “bare metal” stent and you are a high bleeding risk, your health care professional may give you a P2Y12 inhibitor for a shorter period to decrease the chances of bleeding. If you are at a lower risk of bleeding, you may have been treated with a drug-eluting stent, and you may be on DAPT for 6-12 months or longer. If you don’t have a high bleeding risk, a longer duration may lower your risk of future heart attack and clotting of the stent. It’s important to take the medication as prescribed. Stopping it on your own can increase risk of clots forming inside the stent, particularly in the first few months.
- If you had CABG, you may be treated with a P2Y12 inhibitor for a year after the surgery.
If you have questions about your treatment, talk to your primary health care professional.
Angiotensin-converting enzyme (ACE) inhibitors
Some commonly prescribed include:
- Benazepril
- Captopril
- Enalapril
- Fosinopril
- Lisinopril
- Moexipril
- Perindopril
- Quinapril
- Ramipril
- Trandolapril
What the medication does
- Relax and widen blood vessels
- Lower blood pressure
- Make it easier for the heart to pump blood
Reason for medication
- Used to treat or improve symptoms of cardiovascular conditions including high blood pressure and heart failure.
- They also provide health benefits to people who have had a heart attack.
Angiotensin II receptor blockers (or inhibitors)
(Also known as ARBs)
Some commonly prescribed include:
- Azilsartan
- Candesartan
- Eprosartan
- Irbesartan
- Losartan
- Olmesartan
- Telmisartan
- Valsartan
What the medication does
- Relax and widen blood vessels
- Lower blood pressure
- Make it easier for the heart to pump blood
Reason for medication
- Used to treat or improve symptoms of cardiovascular conditions including high blood pressure, heart failure and chronic kidney disease.
Beta blockers
(Also known as Beta-adrenergic blocking agents)
Some commonly prescribed include:
- Acebutolol
- Atenolol
- Betaxolol
- Bisoprolol
- Metoprolol
- Nadolol
- Propranolol
- Sotalol
What the medication does
- May lower blood pressure
- Slow the heart rate (how fast the heart beats)
- Make it easier for the heart to pump blood
Reason for medication
- Used to treat some types of heart attacks, high blood pressure, chest pain (angina) caused by reduced blood supply to the heart muscle and some arrhythmias (abnormal heart rhythms).
- Used to help prevent future heart attacks in people who have had a heart attack.
Combined alpha and beta-blockers
Combined alpha and beta-blockers are used to treat high blood pressure and heart failure.
Some commonly prescribed include:
- Carvedilol
- Labetalol
A possible side effect of combined alpha and beta-blockers:
- May cause a drop in blood pressure when you stand up.
Calcium channel blockers
(Also known as calcium antagonists or calcium blockers)
Some commonly prescribed include:
- Amlodipine
- Diltiazem
- Felodipine
- Nifedipine
- Nimodipine
- Nisoldipine
- Verapamil
What the medication does
May decrease the heart’s pumping strength and relax blood vessels.
Reason for medication
- Used to treat high blood pressure, chest pain (angina) caused by reduced blood supply to the heart muscle and some abnormal heart rhythms.
Cholesterol-lowering medications
Some commonly prescribed include:
- Statins: Atorvastatin, Fluvastatin, Lovastatin, Pitavastatin, Pravastatin, Rosuvastatin, Simvastatin
- Nicotinic acids: Niacin
- Cholesterol absorption inhibitor: Ezetimibe
- Combination statin and cholesterol absorption inhibitors: Ezetimibe/Simvastatin
- Bile acid sequestrants: Cholestyramine, Colesevelam, Colestipol
- PCSK9 inhibitors: Alirocumab, Evolocumab
What the medication does
Various medications can lower blood cholesterol levels. But statins are the best first course of action. When statins don’t work, or if a person has serious side effects from statin therapy, other drugs may be used.
Cholesterol-lowering medications work in the body in different ways. Some affect the liver, some work in the intestines and some interrupt the formation of cholesterol from circulating in the blood.
Reason for medication
Used to lower LDL ("bad") cholesterol.
*Some cholesterol-lowering medications may interact with grapefruit, grapefruit juice, pomegranate and pomegranate juice. Please talk to your health care professional about any potential risks.
Diuretics
(Also known as water pills)
Some commonly prescribed include:
- Acetazolamide
- Amiloride
- Bumetanide
- Chlorothiazide
- Chlorthalidone
- Furosemide
- Hydro-chlorothiazide
- Indapamide
- Metolazone
- Spironolactone
- Torsemide
What the medication does
Causes the body to rid itself of excess fluids and sodium through urination. Helps to reduce the heart's workload. Also decreases the buildup of fluid in the lungs and other parts of the body, such as the ankles and legs. Different diuretics remove fluid at varied rates and through different methods.
Reason for medication
- Used to help lower blood pressure.
- Reduce swelling (edema) from excess buildup of fluid in the body.
Vasodilators
Some commonly prescribed include:
- Isosorbide dinitrate
- Isosorbide mononitrate
- Hydralazine
- Nitroglycerin
- Minoxidil
What the medication does
Widens the blood vessels so the blood flows more easily. Reduces the heart’s workload and decreases blood pressure.
A type of vasodilators called nitrates increases the supply of blood and oxygen to the heart while reducing its workload. This can ease chest pain (angina). Nitroglycerin is available as a pill to be swallowed or absorbed under the tongue, a spray and as a topical cream.
Reasons for medication include
- Used to ease chest pain (angina)
- Used to treat heart attack
- Used to treat high blood pressure
- Treats high blood pressure caused by pregnancy
Surgery or other procedures
Devices for Heart Failure
Implantable cardioverter defibrillator (ICD)
Some people who have severe heart failure or serious arrhythmias (irregular heartbeats) might need implantable cardioverter defibrillators, or ICDs. These devices are surgically placed and detect life-threatening arrhythmias. When they do, they deliver a shock to the heart to reset its rhythm so it can resume normally. Some newer pacemakers can also work as ICDs.
ICDs have saved millions of lives but are only advisable in certain circumstances. The physician and patient share the decision to use an ICD.
Cardiac Resynchronization Therapy (CRT)
Some people with heart failure develop abnormal heart beats, called arrhythmias. This can reduce how well the heart’s lower chambers (ventricles) can function. Cardiac resynchronization therapy, also known as biventricular pacing, may be needed. In this procedure, a special pacemaker makes the ventricles contract at the same time. This helps the lower heart chambers pump and relax together.
This therapy can improve heart function, reduce hospitalization risk and increase survival.
Left ventricular assist device (LVAD)
The left ventricle is the large, muscular chamber of the heart that pumps blood out to the body. An LVAD is a mechanical pump-type device. Some people use this device permanently, but it’s most often considered a bridge to transplant, or a short-term fix if surgery or a heart transplant is needed.
Surgical procedures for heart failure
Surgery isn’t frequently used to treat heart failure. But your health care team might recommend it when they identify a correctable problem that’s causing heart failure, such as a defect, including a heart valve or a blocked coronary artery.
Surgery may also be needed if heart failure is so severe that it can’t be helped with medications and lifestyle changes.
Heart transplantation
Some people have severe, progressive heart failure that can’t be helped by medications, other devices and procedures, or eating and lifestyle changes. In such cases, a heart transplant could be the only effective treatment option.
Surgeons replace the damaged heart with a healthy one from a donor who has identified themselves as an organ donor while alive and been declared brain dead. It can take several months to find a donor heart that closely matches the tissues of the person receiving the transplant. But this matching process is essential to reduce the chances of rejection.
During a transplant procedure, the surgeon connects the patient to a heart-lung machine, which takes over the functions of the heart and lungs. The surgeon then removes the diseased heart and replaces it with the donor heart. Finally, the major blood vessels are reconnected, and the new heart is ready to work.
The outlook for people with heart transplants is good after the transplant. In fact, about 90% of patients live for more than a year after their operations and on average, survival is greater than 12 years. However, the number of patients who receive heart transplants is still relatively low, around 3,500 each year.
Percutaneous coronary intervention (PCI, also referred to as angioplasty)
Heart failure can develop when blockages in the coronary arteries restrict the blood supply to the heart muscle. Removing these blockages can improve overall heart function, which can improve or resolve heart failure symptoms. PCI, often called angioplasty, is one procedure to reopen blocked blood vessels.
The procedure is usually performed in the cardiac catheterization lab. A small tube (catheter) with a tiny, deflated balloon on the end is inserted through an incision in the groin (or other area where the artery can be accessed) and pushed through to the diseased artery. Then the balloon is inflated to push open the artery. The balloon is removed once the artery has been fully opened.
A stent can be placed during the procedure to keep the blood vessel open.
Although there’s a slight risk of damage to the artery during PCI, this procedure usually improves the patient’s condition.
Coronary artery bypass
Coronary artery bypass surgery reroutes the blood supply around a blocked section of the artery.
During this procedure, surgeons remove healthy blood vessels from another part of the body, such as a leg, wrist or the chest wall. They then surgically attach the vessels to the diseased artery so that the blood can flow around the blocked section.
After a bypass operation, it’s especially important to reduce the amount of fat and cholesterol you eat because these substances cause the arteries to clog. Health care professionals also recommend increasing physical activity to strengthen the heart muscles.
Valve replacement
Heart failure is sometimes caused by a defective or diseased heart valve.
Heart valves regulate the flow of blood inside the heart. When the valves don’t work properly, this puts extra strain on the heart and can lead to heart failure.
For some valve problems, medical management is the first step in treatment. Correcting the problem surgically often improves or resolves the condition as well.
During valve repair, the damaged sections of the valve are strengthened. During valve replacement, the failing valve is removed, and a new valve is used in its place. A variety of different replacement valves can be used, including a mechanical valve made from metal and plastic, or one made from human or animal tissue. During the surgery, the patient is connected to a heart-lung machine that supplies blood to the brain and body.
After the operation and depending on the type of replacement heart valve used, patients can take medicines to prevent blood clots from forming around the new heart valve. This treatment is often long-term to ensure the new valve works properly. Most heart valve surgeries are a success, but the operation is only considered as an option when a defective or diseased valve threatens someone’s life.
In some patients, heart valve replacement can occur without surgery. TAVR is a minimally invasive procedure where a new valve is inserted without removing the old, damaged valve. But candidacy for this kind of procedure is highly individualized.
What is cardiac rehabilitation?
Cardiac rehabilitation is an important program for anyone recovering from a heart attack. This can also include heart failure, or some types of heart surgery.
Cardiac rehabilitation is a supervised program that includes
- Physical activity.
- Education about healthy eating.
- Taking medicine as prescribed.
- Ways to help you quit smoking.
- Counseling to find ways to relieve stress and improve mental health.
A team of people may help you through cardiac rehabilitation.
This may include
- Your health care team.
- Exercise and nutrition specialists.
- Physical therapists.
- Counselors or mental health professionals.
How can you prevent heart disease?
The best way to prevent heart disease is to adopt heart-healthy habits. These include managing blood pressure and cholesterol levels, eating a plant-based diet, adopting regular exercise, maintaining a proper weight, getting enough sleep, and not smoking.
Blood pressure. High blood pressure makes the heart work harder, which can weaken the heart muscle over time. Blood pressure is measured in millimeters of mercury (mm Hg) and is categorized as follows:
- Normal: less than 120/80 mm Hg
- Elevated: 120/less than 80 to 129/less than 80 mm Hg
- Stage 1 hypertension: 130/80 to 139/89 mm Hg
- Stage 2 hypertension: 140/90 mm Hg and above.
Cholesterol. There are two main types: "bad" low-density lipoprotein (LDL) and "good" high-density lipoprotein (HDL). Ideally, most adults should keep their LDL below 100 milligrams per deciliter (mg/dL) and their HDL above 40 mg/dL. However, your ideal numbers may differ based on your health, risk factors for heart disease, and individual goals, as determined in consultation with your doctor.
Diet. Following a plant-based diet is known to protect against heart disease. The plant diets that have been most studied for heart health are the Mediterranean diet and the DASH (Dietary Approaches to Stop Hypertension) diet. Each emphasizes eating foods associated with heart-healthy benefits, such as whole grains, fruits, vegetables, legumes, nuts and seeds, fatty fish, and healthy oils like olive oil, and reducing the intake of red meat and processed foods.
Exercise. Guidelines recommend that adults engage in at least 150 minutes of moderate-intensity aerobic activity per week, which breaks down to 30 minutes daily, five days a week. But this is the minimum. Evidence suggests that doing more is better.
Weight. About 30% of American adults are classified as overweight. While it's natural for people's weight to increase somewhat with age, even five to 10 pounds over your ideal number is associated with an increased risk of heart disease. Check with your doctor to determine your weight range for your gender, age, and body type.
Sleep. Experts recommend that adults get at least seven hours of sleep per night. Studies have found that less than this amount is associated with heart disease risk factors like higher stress levels, increased inflammation, high blood pressure, and weight gain.
Smoking. Smokers have a much higher heart disease risk than never-smokers, and two to three times the risk of early death. Certain medications and nicotine replacement therapies can help people quit. Speak with your doctor about these or other options.
Heart Disease Facts
Heart disease in the United States
In the United States:
- Heart disease is the leading cause of death for men, women, and people of most racial and ethnic groups.
- One person dies every 33 seconds from cardiovascular disease.
- In 2022, 702,880 people died from heart disease. That's the equivalent of 1 in every 5 deaths.
- Heart disease cost about $252.2 billion from 2019 to 2020. This includes the cost of health care services, medicines, and lost productivity due to death.
- the top 10 states with the highest heart disease death rates per 100,000 residents were:
- Oklahoma (264.2)
- Mississippi (255.2)
- Alabama (247.5)
- Louisiana (235.5)
- Arkansas (231)
- Tennessee (223.8)
- West Virginia (223)
- Kentucky (217.5)
- Michigan (209.6)
- Nevada (208.1)
- the 10 states with the lowest heart disease rates per 100,000 residents were:
- North Dakota (152.8)
- Florida (151.3)
- Oregon (148.5)
- California (147.8)
- Washington (147.7)
- Connecticut (136.7)
- Colorado (135.1)
- Massachusetts (134)
- Hawaii (126.5)
- Minnesota (123.9)
Coronary artery disease (CAD)
- Coronary heart disease is the most common type of heart disease. It killed 371,506 people in 2022.
- About 1 in 20 adults age 20 and older have CAD (about 5%).
- In 2022, about 1 out of every 5 deaths from cardiovascular diseases (CVDs) was among adults younger than 65 years old.
Heart attack
- In the United States, someone has a heart attack every 40 seconds.
- Every year, about 805,000 people in the United States have a heart attack. Of these, 605,000 are a first heart attack, and 200,000 happen to be people who have already had a heart attack.
- About 1 in 5 heart attacks are silent—the damage is done, but the person is not aware of it.
Did you know?
Early action is important for heart attack. Know the warning signs and symptoms of a heart attack.
As plaque builds up in the arteries of a person with heart disease, the inside of the arteries begins to narrow, which lessens or blocks the flow of blood.
Who is affected
Heart disease deaths vary by sex, race, and ethnicity
Heart disease is the leading cause of death for people of most racial and ethnic groups in the United States. These include African American, American Indian, Alaska Native, Hispanic, and White men. For women from the Pacific Islands and Asian American, American Indian, Alaska Native, and Hispanic women, heart disease is second only to cancer.
Below are the percentages of all deaths caused by heart disease in 2021, listed by ethnicity, race, and sex.
| Race or Ethnic Group | % of Deaths |
| American Indian or Alaska Native | 15.5 |
| Asian | 18.6 |
| Black (Non-Hispanic) | 22.6 |
| Native Hawaiian or Other Pacific Islander | 18.3 |
| White (Non-Hispanic) | 18.0 |
| Hispanic | 11.9 |
| All | 17.4 |
Prognosis
What can I expect if I have heart disease?
Medications and/or procedures can help people who have various types of heart disease. It’s easier to treat most types of heart disease if you get an early diagnosis instead of waiting for symptoms to get worse. Many people can live full lives when they follow their healthcare provider’s treatment plan.
Living With
How do I take care of myself?
If you have coronary artery disease (the most common kind of heart disease), you can improve your health by making changes to your daily life. This may include reducing how much salt and saturated fat you eat and increasing how much you exercise. In addition, a provider may recommend taking medicine to lower your cholesterol and/or blood pressure.
When should I see my healthcare provider?
If you have a biological family history of heart disease, you may want to ask your provider if you have other risk factors. If you do, you can make a plan to help prevent heart disease.
Contact your provider if you have heart disease symptoms.
When should I go to the ER?
Call your local emergency number if you suddenly experience these issues:
- Chest pain, pressure, heaviness or discomfort.
- Fainting.
- Shortness of breath.
What questions should I ask my doctor?
You may want to ask your healthcare provider:
- What kind of heart disease do I have?
- Is my family at risk for this type of disease?
- What’s the best treatment for my situation?
One Final Note..
Your heart has a crucial job, so it’s important to pay attention to warning signs of a heart issue. Many heart diseases develop over time. Identifying heart disease early gives you the best chance of managing it well. Talk with a healthcare provider about the best ways to prevent heart disease or keep it from getting worse. Even if you have risk factors you can’t change, there are other things you have the power to change.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 - K. Kerr Most recent revision February 09, 2026 07:44:10 AM
|