- Main Page
- A1C Test
- Aliens
- American Flag
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation
- Avoiding Scams
- Awareness Ribbons
- Bamboo
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birthday on Planets
- Birth Month
- Blood Pressure - High
- Blood Pressure - Low
- Blood Tests
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Boot Anatomy
- Boot Fit Guide
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- CGM's
- Chakras
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Color Codes Chart
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- C.P.A.P.
- Credit Score Checkers
- Crystals & Gems
- CT scan
- Degenerative Disk Disease
- Depression
- Diabetes Info.
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Dream Catchers
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Emphysema
- Epsom Salt
- Eye Teasers
- Fairies
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Friend
- Funny Things
- Fun Stuff
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Tests
- Hello!!
- Herbal Codes
- Herbology
- Herb & Oils Uses
- Herniated disk
- Home Remedies
- House Plants
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Important Numbers
- Insomnia
- Insulin
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Cleanse
- Logger vs Lineman Boots
- Macaroni!!
- Medicare
- Mental Health
- MO HealthNet
- Moon Phases
- Motorcycle Manufacturers
- Mounjaro®
- MRI Scan
- My Athletic Shoes
- My Boots & Spurs
- My Cowboy Hats
- Myelography
- Mystical Unicorn
- Nasal Polyps
- Natal Astrology Chart
- Never Forget
- Nuclear Medicine
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Gifts
- PVC's
- Quit Smoking
- Recipes I like
- Red Yeast Rice
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Superstitions
- Symbols
- Tarot
- The Ten Commandments
- Tools of the Craft
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Tree, Calamondin Orange
- Tree, Lemon (Meyer)
- Tree, Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- Vaccines by Age
- Vaccines - Adults
- Vaccines - Kids
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamins & Minerals
- Water Therapy
- Wiccan Rede
- X-rays
- Yin / Yang
- Zodiac Signs
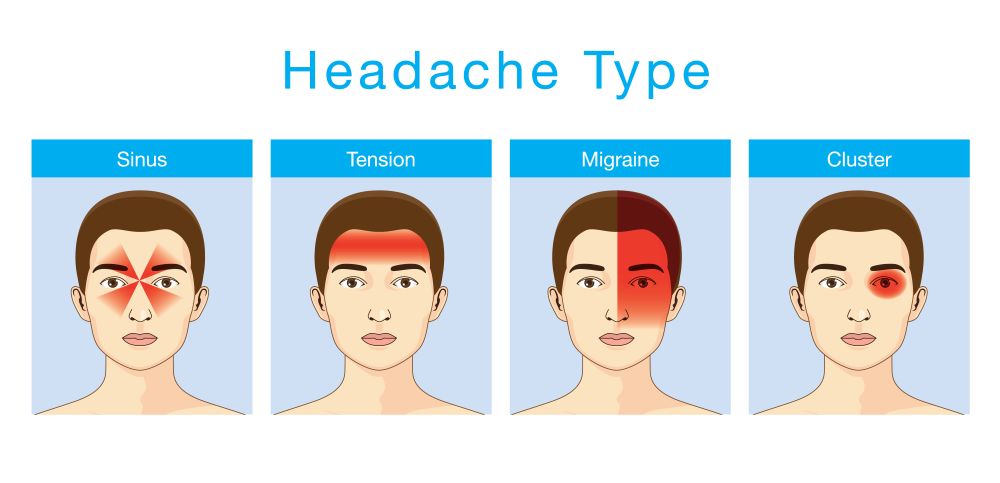
Headaches
Overview
Headaches are a very common condition that most people will experience many times during their lives. The main symptom of a headache is pain in your head or face. There are several types of headaches, and tension headaches are the most common. While most headaches aren’t dangerous, certain types can be a sign of a serious underlying condition.
Headache is pain in any region of the head. Headaches may occur on one or both sides of the head, be isolated to a certain location, radiate across the head from one point, or have a viselike quality.
A headache may appear as a sharp pain, a throbbing sensation or a dull ache. Headaches can develop gradually or suddenly, and may last from less than an hour to several days.
What is a headache?
A headache is a pain in your head or face that’s often described as a pressure that’s throbbing, constant, sharp or dull. Headaches can differ greatly in regard to pain type, severity, location and frequency.
Headaches are a very common condition that most people will experience many times during their lives. They’re the most common form of pain and are a major reason cited for days missed at work or school, as well as visits to healthcare providers.
While most headaches aren’t dangerous, certain types can be a sign of a more serious condition.
What are the types of headaches?
There are more than 150 types of headaches. They fall into two main categories: primary and secondary headaches.
Primary headaches
Dysfunction or over-activity of pain-sensitive features in your head cause primary headaches. They’re not a symptom of or caused by an underlying medical condition. Some people may have genes that make them more likely to develop primary headaches.
Types of primary headaches include:
- Tension-type headaches (most common type of headache).
- Migraine headaches.
- Migraine with aura
- Cluster headache
- Trigeminal autonomic cephalalgia (TAC), such as cluster headache and paroxysmal hemicrania
- New daily persistent headaches (NDPH).
Some primary headaches can be triggered by lifestyle factors or situations, including:
- Alcohol, particularly red wine.
- Certain foods, such as processed meats that contain nitrates (food-triggered headaches).
- Consuming nicotine (nicotine headache).
- Changes in sleep or lack of sleep.
- Sex headaches
- Poor posture.
- Physical activity, such as exercise (exertion headaches).
- Skipped meals (hunger headache).
- Coughing, sneezing, blowing your nose, straining (such as when having a bowel movement), or laughing or crying vigorously (cough headaches).
Primary headaches typically aren’t dangerous, but they can be very painful and disrupt your day-to-day life.
Secondary headaches
An underlying medical condition causes secondary headaches. They’re considered a symptom or sign of a condition.
Types of secondary headaches that aren’t necessarily dangerous and resolve once the underlying condition is treated include:
- Dehydration headache.
- Sinus headaches.
- Medication overuse headaches.
Types of secondary headaches that can be a sign of a serious or potentially life-threatening condition include:
Spinal headaches: Spinal headaches are intense headaches that occur when spinal fluid leaks out of the membrane covering your spinal cord, usually after a spinal tap. Most spinal headaches can be treated at home, but prolonged, untreated spinal headaches can cause life-threatening complications, including subdural hematoma and seizures.
Thunderclap headaches: A thunderclap headache is an extremely painful headache that comes on suddenly, like a clap of thunder. This type of headache reaches its most intense pain within one minute and lasts at least five minutes. While thunderclap headaches can sometimes be harmless, it’s important to seek immediate medical attention. They can be a sign of:
- Head injury.
- Brain bleed.
- Reversible cerebral vasoconstriction syndrome.
- A sudden, severe rise in blood pressure.
What’s the difference between a headache and a migraine?
A migraine is a type of primary headache disorder.
A migraine is a common neurological condition that causes a variety of symptoms, most notably a throbbing headache on one side of your head. Migraines often get worse with physical activity, lights, sounds or smells. They usually last at least four hours or even days.
Who do headaches affect?
Anyone can have a headache, including children, adolescents and adults. About 96% of people experience a headache at least once in their life.
About 40% of people across the world have tension-type headaches and about 10% have migraine headaches.
Symptoms and Causes
What is the main cause of a headache?
Headache pain results from signals interacting among your brain, blood vessels and surrounding nerves. During a headache, multiple mechanisms activate specific nerves that affect muscles and blood vessels. These nerves send pain signals to your brain, causing a headache.
Are headaches hereditary?
Headaches tend to run in families, especially migraines. Children who have migraines usually have at least one biological parent who also experiences them. In fact, kids whose parents have migraines are up to four times more likely to develop them.
Headaches can also be triggered by environmental factors shared in a family’s household, such as:
- Eating certain foods or ingredients, like caffeine, alcohol, fermented foods, chocolate and cheese.
- Exposure to allergens.
- Secondhand smoke.
- Strong odors from household chemicals or perfumes.
What headache symptoms require immediate medical care?
If you or your child has any of these headache symptoms, get medical care right away:
- A sudden, new and severe headache.
- Headache with a fever, shortness of breath, stiff neck or rash.
- Headaches that occur after a head injury or accident.
- Getting a new type of headache after age 55.
Also seek medical care right away if your headache is associated with neurological symptoms, such as:
- Weakness.
- Dizziness.
- Sudden loss of balance or falling.
- Numbness or tingling.
- Paralysis.
- Speech difficulties.
- Mental confusion.
- Seizures.
- Personality changes/inappropriate behavior.
- Vision changes (blurry vision, double vision or blind spots).
When to see a doctor
Seek emergency care
A headache can be a symptom of a serious condition, such as a stroke, meningitis or encephalitis.
Go to a hospital emergency room or call 911 or your local emergency number if you're experiencing the worst headache of your life, a sudden, severe headache or a headache accompanied by:
- Confusion or trouble understanding speech
- Fainting
- High fever, greater than 102 F to 104 F (39 C to 40 C)
- Numbness, weakness or paralysis on one side of your body
- Stiff neck
- Trouble seeing
- Trouble speaking
- Trouble walking
- Nausea or vomiting (if not clearly related to the flu or a hangover)
Schedule a doctor's visit
See a doctor if you experience headaches that:
- Occur more often than usual
- Are more severe than usual
- Worsen or don't improve with appropriate use of over-the-counter drugs
- Keep you from working, sleeping or participating in normal activities
- Cause you distress, and you would like to find treatment options that enable you to control them better
Diagnosis and Tests
How are headaches evaluated and diagnosed?
If you have headaches often or if they’re very severe, reach out to your healthcare provider.
It’s important to diagnose headaches correctly so your provider can prescribe specific therapy to help you feel better. Your provider will complete a physical examination, discuss your medical history and talk to you about your headache symptoms. This conversation is part of a headache evaluation.
During the headache evaluation, your provider will ask you about your headache history, including:
- What the headaches feel like.
- How often the headaches happen.
- How long the headaches last each time.
- How much pain the headaches cause you.
- What foods, drinks or events trigger your headaches.
- How much caffeine you drink each day.
- What your stress level is.
- What your sleep habits are like.
Your headache can be more accurately diagnosed by knowing:
- When the headache started.
- Whether there’s a single type of headache or multiple types of headaches.
- If physical activity aggravates the headache pain.
- Who else in your family has headaches.
- What symptoms, if any, occur between headaches.
After completing the medical history part of the evaluation, your provider may perform physical and neurological examinations. They’ll look for signs and symptoms of an illness or condition that may be causing the headache, including:
- Fever.
- Infection.
- High blood pressure.
- Muscle weakness, numbness or tingling.
- Excessive fatigue.
- Loss of consciousness.
- Balance problems and frequent falls.
- Vision problems (blurry vision, double vision, blind spots).
- Mental confusion or personality changes.
- Seizures.
- Dizziness.
- Nausea and vomiting.
Neurological tests focus on ruling out diseases that might also cause headaches. A disorder of your central nervous system might be suspected in the development of serious headaches.
After evaluating the results of your headache history, physical examination and neurological examination, your physician should be able to determine what type of headache you have, whether or not a serious problem is present and whether additional tests are needed.
If they’re unsure of the cause, they may refer you to a headache specialist.
What tests will be done to diagnose headaches?
Although scans and other imagining tests can be important when ruling out other diseases, they don’t help in diagnosing migraines, cluster or tension-type headaches.
But if your healthcare provider thinks that your headaches are being caused by another medical condition, there are several imaging tests they may order.
A CT scan or MRI can help determine if your headaches are connected to an issue with your central nervous system. Both of these tests produce cross-sectional images of your brain that can show any abnormal areas or problems.
Management and Treatment
How is a headache treated?
Treatment for headaches depends on the type.
One of the most crucial aspects of treating primary headaches is figuring out your triggers. Learning what those are — typically by keeping a headache log — can reduce the number of headaches you have.
Once you know your triggers, your healthcare provider can tailor treatment to you. For example, you may get headaches when you’re tense or worried. Counseling and stress management techniques can help you handle this trigger better. By lowering your stress level, you can avoid stress-induced headaches.
Not every headache requires medication. A range of treatments is available. Depending on your headache type, frequency and cause, treatment options include:
- Stress management.
- Biofeedback.
- Medications.
- Treating the underlying medical condition/cause.
Stress management for headache
Stress management teaches you ways to cope with stressful situations. Relaxation techniques help manage stress. You use deep breathing, muscle relaxation, mental images and music to ease your tension.
Biofeedback for headache
Biofeedback teaches you to recognize when tension is building in your body. You learn how your body responds to stressful situations and ways to settle it down. During biofeedback, sensors are connected to your body. They monitor your involuntary physical responses to headaches, which include increases in:
- Breathing rate.
- Pulse.
- Heart rate.
- Temperature.
- Muscle tension.
- Brain activity.
Medications for headache
Occasional tension headaches usually respond well to over-the-counter pain relievers. But be aware that using these medications too often can lead to long-term daily headaches (medication overuse headaches).
For frequent or severe headaches, your provider may recommend prescription headache medications. Triptans and other types of drugs can stop a migraine attack. You take them at the first signs of an oncoming headache.
Drugs for high blood pressure, seizures and depression can sometimes prevent migraines. Your healthcare provider may recommend trying one of these medications to reduce headache frequency.
Treating the underlying medical condition causing secondary headache
Treatment for secondary headaches involves treating the underlying medical condition causing it.
For example, surgery is often needed to correct the underlying cause of secondary cough headache.
How can I get rid of a headache?
You can treat the occasional, mild headache at home with over-the-counter pain relievers. Other self-care treatments for headaches include:
- Applying heat or cold packs to your head.
- Doing stretching exercises.
- Massaging your head, neck or back.
- Resting in a dark and quiet room.
- Taking a walk.
Prevention
How can I prevent headaches?
The key to preventing headaches is figuring out what triggers them. Triggers are very specific to each person — what gives you a headache may not be a problem for others. Once you determine your triggers, you can avoid or minimize them.
For example, you may find that strong scents set you off. Avoiding perfumes and scented products can make a big difference in how many headaches you have. The same goes for other common triggers like troublesome foods, lack of sleep and poor posture.
Many people, however, aren’t able to avoid triggers or are unable to identify triggers. In that case, a more personalized multidisciplinary approach with a headache specialist is often necessary.
Prognosis
Can headaches or migraines be cured?
Treating health problems that cause headaches, such as high blood pressure, can eliminate head pain. Recently, there have been several new advancements in our understanding of what causes headaches.
Although researchers are closer than ever before to a cure, at this time, there isn’t a cure for primary headaches. Treatment focuses on relieving symptoms and preventing future episodes.
Living With Headaches
When should I see my healthcare provider about headaches?
Contact your healthcare provider if you or your child has any of the following symptoms or situations:
- Experiencing one or more headaches per week.
- Experiencing headaches that keep getting worse and won’t go away.
- Needing to take a pain reliever every day or almost every day for your headaches.
- Needing more than two to three doses of over-the-counter medications per week to relieve headache symptoms.
- Experiencing headaches that are triggered by exertion, coughing, bending or strenuous activity.
- Having a history of headaches but experiencing a recent change in your headache symptoms.
One Final Note..
If your headaches are interfering with your daily functioning or affecting your mood, it’s important to talk to your healthcare provider. If possible, try to write down how you feel when you’re experiencing a headache. Keeping a journal of your headaches and how they make you feel can be helpful when you’re talking to your provider.
The information you give your healthcare provider about your headaches is the most important part of the diagnosis process. By giving your provider as much information as possible about your headaches, you’re more likely to get an accurate diagnosis and treatment plan that will help you feel better.
Find me on Social Media
 |
Don't forget to bookmark my site to see updates.. Copyright © 2000 - 2025 K.
Kerr |






