- Main Page
- A1C Test
- Advance Directives
- Age on other Planets
- Aliens
- American Flag
- Angels
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Aphrodisiacs
- Arrhythmia
- Atrial Fibrillation
- Auras
- Avoiding Scams
- Awareness Ribbons
- Baileys Liqueur
- Bananas
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birth Month
- Blood Tests
- Blood Test Tubes
- Blood Types
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Book of Shadows
- Book List
- Boot Anatomy
- Boot Fit Guide - Cowboy
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Bullying
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- Cats
- CGM's
- Chakras
- Chillicothe Businesses
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Ciroc Vodka
- Citalopram
- Coffee Pods
- Color Codes Chart
- Consumer Resources
- Consumer Resources - Elders
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hats
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- Cowboy Sites
- C.P.A.P.
- Craft Name!
- Credit Score Checkers
- Credit Scores
- Crystals & Gems
- CT scan
- Cyclobenzaprine
- Degenerative Disc Disease
- Deities
- Depression
- Diabetes Info.
- Diabetes Facts
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Disability Permits
- Disaronno Amaretto
- Do Not Resuscitate
- Donation
- Dream Catchers
- Dreams
- Drug Test
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Electromyography
- Elementals
- Elements
- Emphysema
- Epsom Salt
- Eye Teasers
- Facet Arthropathy
- Fairies
- Fairies of Folklore
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Fortune Teller
- Free For All Links
- Friend
- Funny Things
- Fun Stuff
- Gabapentin
- GERD
- Giving
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Healing & Energy Work
- Health Facts
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Imaging Tests
- Hello!!
- Herbal Codes
- Herbal Medicine
- Herb & Oils Uses
- Herniated disc
- HIPAA
- Home Bar
- Home Remedies
- Horse Sites
- House Plants
- Humalog®
- Hunger Facts
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hyperlipidemia
- Hypertension
- Hypotension
- Important Numbers
- Indomethacin
- Informed Consent
- Inhalers
- Insomnia
- Insulin
- Interesting Facts
- Juice Fasting
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Benefits
- Lime Benefits
- Logger vs Lineman
- Lucky Bamboo
- Lumbar Retrolisthesis
- Macaroni!!
- Magic 8 Ball
- Magick
- Medicaid
- Medicare
- Melatonin
- Men's Health
- Mental Health
- Mirror Messages
- Missouri
- Missouri Prisons
- MO HealthNet
- Moon Phases
- Mounjaro®
- MRI Scan
- Muses
- Myelography
- Mystical Unicorn
- Naproxen
- Nasal Polyps
- Natal Astrology Chart
- National Foundations
- Need a Spell?
- Never Forget
- New Page Soon
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Otolaryngologist
- Ouija
- Oxycodone-Acetaminophen
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- PET/CT Scan
- PET Scan
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Dictionary
- Psychic Gifts
- Psychic Reader
- Psychic Scams
- Psychic Test
- Psychometry
- PVC's
- Quartz Crystals
- Quetiapine
- Quit Smoking
- Radiculopathy
- Ragtime Music
- Recipes I like
- Red Yeast Rice
- Reiki
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Scam Calls
- Sciatica
- Scrying
- Séance
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- SPECT Scan
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Spirit Guides
- Statins
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Superstitions
- Support Groups
- Symbols
- Talisman
- Tardive Dyskinesia
- Tarot
- Tea Leaf Reading
- Telekinesis
- Tequila Rose
- Testosterone
- The Ten Commandments
- Tools of the Craft
- Top Alcohol
- Top Animated Movies
- Top Comedy Movies
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Trazodone
- Tree, Calamondin Orange
- Tree, Meyer Lemon
- Tree, Persian Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- UV Vodka
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Vaccines 19 and up
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin F
- Vitamin K
- Vitamins & Minerals
- Vitamins Recommended
- Water Benefits
- Weight on other Planets
- Wheel of the Year
- White Magick
- Wicca
- Wiccan Rede
- Wine Clubs
- Wines
- Wines - Missouri
- X-Rays
- Yin / Yang
- Zodiac Signs
Needed to read PDF's
Overweight & Obesity
Overview
Obesity is a big problem worldwide. It means having too much body fat, often checked with the body mass index (BMI). It can cause heart disease, diabetes, and some cancers.
Knowing why and how obesity happens is key to managing weight. Genetics, lifestyle, and environment all play parts. Eating right, watching calories, and exercising help keep weight in check.
This article will dive into what obesity is, how common it is, and why it happens. We’ll also look at ways to manage and prevent it. Our goal is to help people make better health choices.
Defining Obesity and Its Prevalence
Obesity is a serious health condition where too much body fat can cause many health problems. It’s not just about looks; it’s a major health issue affecting millions globally. Doctors use specific tools and criteria to check if someone is obese.
While BMI is helpful, it has its limits. It doesn’t tell the difference between muscle and fat, which can cause errors. Other tools like waist size and body fat percentage offer more insight into obesity risk.
Global and National Obesity Statistics
Obesity has grown a lot in the last few decades, becoming a big health problem worldwide. The World Health Organization says obesity has almost tripled from 1975. In 2016, over 1.9 billion adults were overweight, with more than 650 million obese.
In the U.S., obesity is a big worry. The Centers for Disease Control and Prevention (CDC) says 42.4% of adults were obese in 2017-2018. This shows nearly half of adults in the country are obese, making it critical to find ways to prevent and manage it.
Symptoms and Diagnosis
There are no specific symptoms of overweight and obesity. Your healthcare provider may diagnose overweight and obesity based on your medical history and high body mass index (BMI). Your provider may also order tests to rule out other medical conditions.
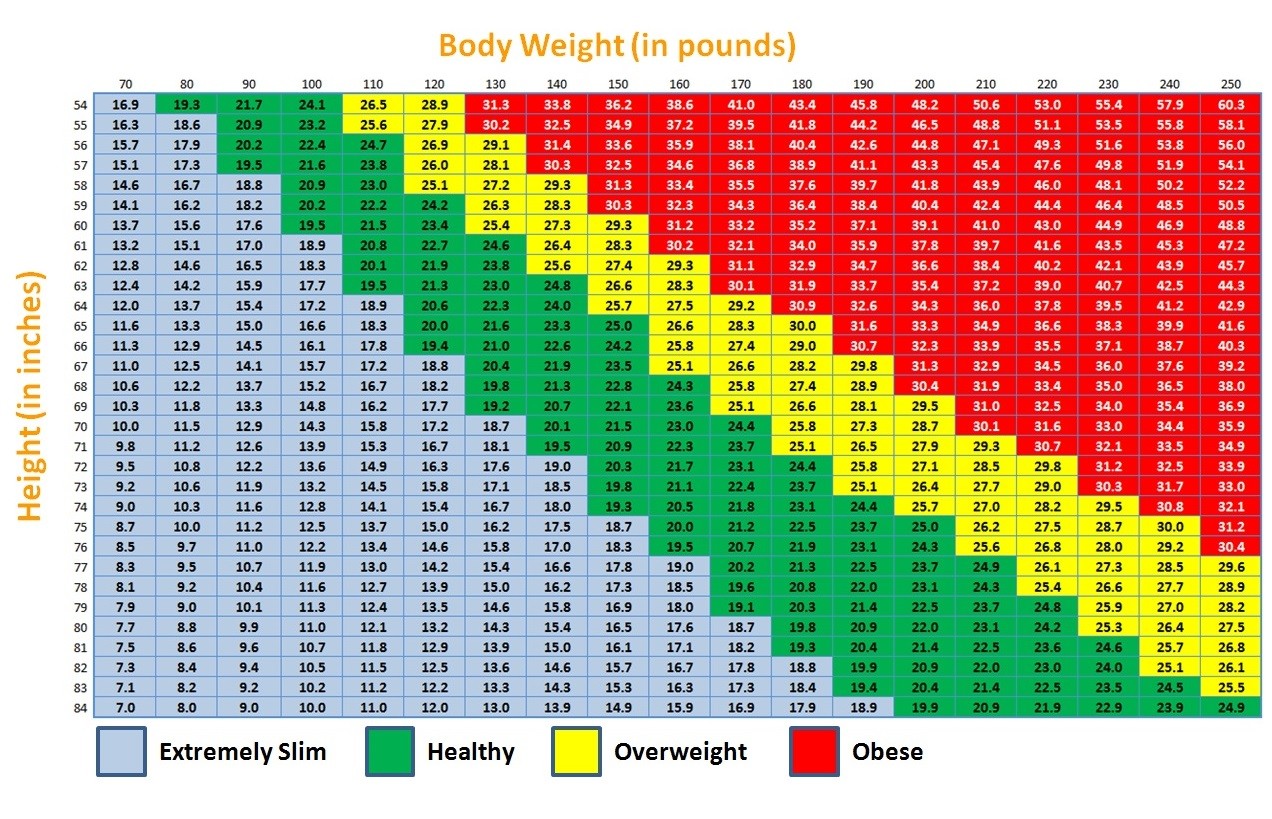
Body mass index
Your BMI is a measure of body fat based on your weight and height. It is important to know that body mass index is a screening tool and does not necessarily diagnose body fatness. Other related measures, such as waist circumference, are used to evaluate a person’s health and risk of overweight and obesity.
BMI categories for adults
For adults:
- Underweight is a BMI of less than 18.5
- Healthy weight is a BMI of 18.5 to 24.9
- Overweight is a BMI of 25 to 29.9
- Obesity is a BMI of 30 or above
Unhealthy body fat distribution
To better understand the health risks that overweight and obesity may pose to a specific person providers can measure the person’s distribution of body fat. You may have a normal BMI but if you have a large waist circumference, you may have more fat in your abdomen than elsewhere.
- For men, an unhealthy waist circumference is greater than 40 inches.
- For women, an unhealthy waist circumference is greater than 35 inches.
Fatty tissue is found in different parts of your body. Fatty tissue produces hormone, cushions your joints, and stores energy.
However, depending on where the fatty tissue is found, it may do more harm than good. Fatty tissue found inside your abdomen is called visceral or abdominal fat. We do not know what causes the body to create and store visceral fat. But we do know that this type of fat interferes with your body’s endocrine and immune systems. It also promotes inflammation and contributes to obesity-related complications, including heart disease and diabetes.
Talk to your healthcare provider about your BMI results and body fat distribution and what steps you may need to take to reach a healthy weight.
Testing for causes of overweight and obesity
Sometimes other medical conditions or medicines that you take may lead to overweight and obesity. These conditions or medicines may disrupt the delicate balance of hormones that control how we use and store energy. Your provider may order blood tests to rule out one of these conditions.
- Cushing’s syndrome is a disorder that happens when your body makes too much of the stress hormone cortisol.
- Hypothyroidism is a condition in which your body does not produce enough thyroid hormone. This slows down your body’s use of energy (food), called metabolism.
- Polycystic ovary syndrome (PCOS) is a condition that affects the ovaries and results in hormone imbalance. PCOS can also be ruled out using ultrasound, a test where sound waves are used to create images of organs.
Talk with your provider if you start gaining or losing weight when you take prescribed medicines.
Click on picture for a full screen view
Prevention
You and your child should each see a healthcare provider once a year to monitor changes in body mass index (BMI). Your provider or your child’s pediatrician may recommend lifestyle changes if BMI regularly increases. This is to prevent you or your child from developing overweight or obesity.
Health Consequences of Obesity
Obesity is a complex condition with many health risks. It can lead to various chronic diseases and obesity complications. People with obesity face a higher risk of serious conditions. These can lower their quality of life and increase healthcare costs.
Some common chronic diseases linked to obesity include:
- Type 2 diabetes
- Cardiovascular disease
- Certain types of cancer
- Sleep apnea
- Osteoarthritis
Excess body weight strains organs, leading to insulin resistance and high blood pressure. These changes can worsen if not treated, increasing health risks.
Obesity also affects mental health, with more depression, anxiety, and low self-esteem. The stigma and discrimination faced by people with obesity can make these issues worse.
| Obesity Complication | Increased Risk |
| Type 2 Diabetes | 5-fold |
| Hypertension | 2.5-fold |
| Coronary Heart Disease | 2-fold |
Dealing with obesity needs a full approach. This includes lifestyle changes, medical help, and support from healthcare and loved ones. By managing weight and adopting healthy habits, people can lower their risk of chronic diseases and improve their well-being.
Causes and Risk Factors
What causes overweight and obesity?
Overweight and obesity can develop over time when you consume more calories than you use. This is also described as an energy imbalance: when your energy in (calories) does not equal your energy out (calories your body uses for things such as breathing, digesting food, and being physically active).
Your body uses certain nutrients, such as carbohydrates or sugars, proteins, and fats, from the foods you eat to make and store energy.
- Food is turned into energy for immediate use to power routine daily body functions and physical activity.
- Food is stored as energy for future use by your body. Sugars are stored as glycogen in the liver and muscles. Fats are stored mainly as triglycerides in fatty tissue.
An energy imbalance causes your body to store more fat than can be used now or in the future. But your risk of developing overweight or obesity is determined by more than how much you eat. It also includes the types and amount of food and drinks you consume each day, your level of physical activity (such as whether you sit at an office desk or are on your feet all day), and how much good-quality sleep you get each night.
All of these factors, as well as many others, can contribute to weight gain.
What raises the risk of overweight and obesity?
There are many risk factors for overweight and obesity. Some are individual factors like knowledge, skills, and behaviors. Others are in your environment, such as school, workplace, and neighborhood. Additionally, food industry practices and marketing as well as social and cultural norms and values can also impact your risk.
You may not be able to change all of your risk factors for overweight or obesity. But knowing your risk is important to help you take steps to reaching a healthy weight and lowering your risk for obesity-related health problems, such as heart disease.
Lack of physical activity
Lack of physical activity, combined with high amounts of TV, computer, video game, or other screen time has been associated with a high body mass index (BMI). Most adults need at least 150 minutes of aerobic activity a week. It is also recommended that adults do muscle-strengthening activities for major muscle groups on 2 or more days each week, as these activities give additional health benefits. Children should get 60 minutes of aerobic activity each day.
Unhealthy eating behaviors
Some unhealthy eating behaviors can increase your risk for overweight and obesity.
- Eating more calories than you use: The number of calories you need will vary based on your sex, age, and physical activity level. Find daily calorie needs or goals for adults as part the DASH Eating Plan.
- Eating too much saturated fat: According to the Dietary Guidelines for Americans, the amount of saturated fat in your daily diet should be no more than 10% of your total calories. For a 2,000-calorie diet, that’s about 200 calories or about 22 grams of saturated fat.
- Eating foods high in added sugar: On a daily basis, try to limit the amount of added sugar in your diet to no more than 10% of your calories.
Not getting enough good-quality sleep
Research has shown a link between poor sleep — not getting enough sleep or not getting enough good-quality sleep — and a high BMI. Regularly getting less than 7 hours of sleep per night can affect the hormones that control hunger urges. In other words, not getting good-quality sleep can make us more likely to overeat or not recognize our body’s signals that we are full.
High amounts of stress
Long-term and even short-term stress can affect the brain and trigger your body to make hormones, such as cortisol, that control energy balances and hunger urges. These hormone changes can make you eat more and store more fat.
Health conditions
Some conditions, such as metabolic syndrome and polycystic ovary syndrome, cause people to gain weight. These medical conditions must be treated for a person’s weight to come close to or into normal range.
Genetics
Some people are predisposed to being heavier. Researchers have found at least 15 genes that influence obesity. Studies show that genetics may play a more important role in people with obesity than in people who are overweight. For people with a genetic high risk for obesity, making healthy lifestyle changes can help lower that risk.
Medicines
Some medicines cause weight gain by disrupting the chemical signals that tell your brain you are hungry.
These include:
- Antidepressants
- Antipsychotics
- Beta-blockers, which are used to treat high blood pressure
- Birth control
- Glucocorticoids, which are often used to treat autoimmune disease
- Insulin, which is a hormone taken to control blood sugar levels in people with diabetes
Talk to your provider if you notice weight gain while you are using one of these medicines. Ask whether there are other forms of the same medicine or other medicines that can treat your medical condition but have less of an effect on your weight.
Your environment
Your environment can contribute to unhealthy eating and a lack of physical activity. Your environment includes all of the parts where you live and work — your home, buildings in which you work or shop, streets, and open spaces. The types of restaurants and the amount of green space you have can contribute to overweight and obesity.
Studies have shown that access to sidewalks and green spaces can help people be more physically active, and grocery stores and farmers markets can help people eat healthier. On the other hand, people living in neighborhoods with more fast food restaurants and inaccessible or no sidewalks or bike paths are more likely to be overweight or obese.
Treatment
If you are diagnosed with overweight or obesity, you and your healthcare provider will work together to develop a treatment plan. Your plan will likely include reducing the number of calories you eat each day, getting more physical activity, and adopting lifelong healthy lifestyle changes.
The goal of your treatment plan is to reduce your risk of obesity-related complications and improve your quality of life. Depending on your body mass index (BMI) and other health conditions you have, your provider may also talk to you about dietary or nutritional counseling, behavioral weight-loss treatment programs, medicines, or surgery. The obesity screening, counseling, and weight-loss programs may be covered by your insurance.
Nutrition and Weight Management
Proper nutrition is key to managing weight and fighting obesity. Eating a balanced diet and controlling portions helps. Making smart healthy food choices also plays a big role.
Balanced Diet and Portion Control
A balanced diet includes many nutrient-rich foods from different groups. It’s also important to limit processed and high-calorie foods. Eating the right amount of food is vital for a healthy weight.
Here’s a guide to help you understand serving sizes:
| Food Group | Recommended Serving Size |
| Fruits | 1 medium piece or 1 cup |
| Vegetables | 1 cup raw or 1/2 cup cooked |
| Grains | 1 slice bread or 1/2 cup cooked |
| Protein | 3 oz cooked lean meat or 1/2 cup cooked beans |
| Dairy | 1 cup milk or yogurt, 1 oz cheese |
Meal Planning and Healthy Food Choices
Meal planning helps keep your diet balanced and portion sizes in check. Preparing meals ahead and choosing wisely ensures you eat well. Here are some tips:
- Choose whole grains over refined ones
- Go for lean proteins like chicken, fish, and beans
- Add a variety of fruits and vegetables to your meals
- Drink less sugary drinks and snacks
- Swap unhealthy fats for healthier ones like avocado and nuts
By focusing on nutrition and using smart weight management strategies, you can reach a healthy weight. This reduces the risk of obesity-related health issues.
Physical Activity and Exercise for Obesity Management
Regular physical activity and exercise are key in managing obesity and losing weight. They help burn extra calories, increase metabolism, and enhance health. The American Heart Association suggests adults do at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise weekly.
Mixing up exercises can make staying active more fun and lasting. Some great exercises for managing obesity include:
| Exercise Type | Benefits |
| Brisk walking | Low-impact, easy to start, improves cardiovascular health |
| Swimming | Low-impact, full-body workout, easy on joints |
| Cycling | Low-impact, builds endurance, strengthens leg muscles |
| Strength training | Builds lean muscle, boosts metabolism, improves bone density |
- Adding more daily physical activity can also help with weight loss and managing obesity. Simple actions like taking the stairs, parking far, or doing chores more vigorously can burn calories over time.
- Before starting any new exercise, it’s important to talk to a healthcare professional, even more so for those with obesity or health issues. Start with low-intensity activities and gradually increase the intensity and duration. This approach helps avoid injuries and ensures long-term success in managing obesity through physical activity and exercise.
- Purchase a scale to weigh yourself here at iHealth Labs Inc
Behavioral weight-loss programs
Research has shown that there are areas of your brain that respond to pleasure. A chemical messenger is released whenever this part of the brain is stimulated by something we enjoy, such as eating food. The stimulation makes us feel good. Research shows that these connections may be stronger in some people than in others, which may explain why some people have a harder time losing weight.
Individual or group behavioral weight-loss programs are run by people who understand these brain connections. In these programs, one or more trained healthcare professionals, such as a registered dietitian and nutritionist (RDN), psychologist, or exercise physiologist, will work with you to develop a customized weight-loss plan. The plan will likely include a reduced-calorie diet, physical activity goals, and behavioral strategies to help you make and maintain these lifestyle changes.
Your weight-loss specialist usually reviews or modifies your goals every 6 months, based on your progress and overall health.
When you are choosing a behavioral weight-loss program, you may want to consider whether the program:
- Offers the service of multiple professionals, such as registered dietitians, doctors, nurses, psychologists, and exercise physiologists
- Provides goals that have been customized for you and that consider things such as the types of food you like, your schedule, your physical fitness, and your overall health
- Provides individual or group counseling to help you change your eating patterns and personal unhealthy habits
- Teaches long-term strategies to deal with problems that can lead to future weight gain, such as stress or slipping back into unhealthy habits
Other things to consider when selecting a program include:
- How many people have successfully completed the program
- The average weight loss for people who finish the program
- Possible side effects or risks
- Fees or costs for additional items, such as dietary supplements
Medicine
When healthy lifestyle changes are not enough, your provider may treat overweight and obesity with medicines. The Food and Drug Administration (FDA) has approved several medicines for weight loss or management.
Pharmacotherapy uses medicines to help manage weight. These drugs can make you feel full, reduce hunger, or change how your body absorbs nutrients. Some common medicines include:
| Medication | Mechanism of Action |
| Orlistat | Reduces fat absorption in the intestines |
| Phentermine | Suppresses appetite by acting on the central nervous system |
| Liraglutide | Mimics a hormone that promotes feelings of fullness |
| Bupropion/Naltrexone | Combination drug that reduces appetite and cravings |
Remember, these medicines work best when used with a healthy diet and exercise. Always talk to your doctor to find the right medicine for you.
Weight-loss medicines are not recommended as a single treatment for weight loss. These medicines can help you lose weight but should be combined with lifestyle changes for greater and longer-lasting weight loss.
Tell your provider about all the medicines you take, because some of these medicines should not be used if you have certain conditions or are taking certain other medicines. Also, these medicines may have side effects. Talk to your provider if you are pregnant, planning to get pregnant, breastfeeding, or have a family history of cardiovascular conditions, such as high blood pressure, heart attack, or stroke.
Devices
The FDA has approved three weight-loss devices for adults. About half the people who undergo procedures to implant these devices lose at least 5% of their initial body weight as a result of the devices.
- Gastric balloons are placed in the stomach via a swallowable capsule attached to a thin catheter or via an endoscope (a long flexible tube with a small camera and a light at the end). Then, depending on the device, the balloons may be filled with gas or liquid (such as salt water) and sealed. Later, they are removed.
- Gastric bands are surgically implanted around the stomach, limiting the amount of food a person can eat at one time and increasing digestion time. This helps people eat less.
- Gastric emptying systems include a tube placed in the stomach via an endoscope and a port that lies against the skin of the abdomen. The tube drains a portion of the stomach contents into a container 20 to 30 minutes after meals. The device is removed when the patient reaches their goal weight.
Your doctor will monitor you for pain, Vitamin deficiencies, anemia, persistent nausea and vomiting, intolerance to solid food, and failure to lose weight. These complications can be treated if they occur.
Surgery
Some people do not lose weight by making healthy lifestyle changes or taking medicines. If your BMI is 35 or greater and you are at risk for obesity-related complications, you may be eligible for surgery if you develop obesity-related complications.
Types of weight-loss (also called bariatric) surgeries are listed below.
- Gastrectomy: A big portion of the stomach is removed to reduce the amount of food that you can eat.
- Gastric banding: The gastric band mentioned above is placed around the upper part of the stomach. This creates a smaller stomach.
- Gastric bypass surgery: A small part of the stomach is connected to the middle part of the intestine, bypassing the first part of intestine. This reduces the amount of food that you can eat and the amount of fat your body can take in and store.
Talk to your doctor to learn more about the benefits and risks of each type of surgery. All surgeries carry some type of risk of possible complications, including bleeding, infection, or even death.
Medications for Obesity
The medications listed below are related to or used in the treatment of this condition.
| Drug name | Rating | Rx/OTC | Preg | CSA | Alcohol |
| phentermine | 8.6 | Rx | X | 4 | X |
| bupropion / naltrexone | 6.6 | Rx | X | N | X |
| Contrave | 6.6 | Rx | X | N | X |
| liraglutide | 7.5 | Rx | C | N | X |
| Saxenda | 7.5 | Rx | C | N | X |
| tirzepatide | 8.8 | Rx | N | X | |
| semaglutide | 7.5 | Rx | N | X | |
| phentermine / topiramate | 7.7 | Rx | X | 4 | X |
| Adipex-P | 8.9 | Rx | X | 4 | X |
| Qsymia | 7.6 | Rx | X | 4 | X |
| Wegovy | 7.5 | Rx | N | X | |
| Mounjaro | 8.9 | Rx | N | X | |
| orlistat | 7.4 | Rx/OTC | X | N | |
| Zepbound | 8.9 | Rx | N | X | |
| topiramate Off-label | 7.3 | Rx | D | N | X |
| diethylpropion | 8.7 | Rx | B | 4 | X |
| phendimetrazine | 8.2 | Rx | C | 3 | X |
| Xenical | 8.2 | Rx | X | N | |
| Alli | 6.1 | OTC | X | N | |
| bupropion Off-label | 7.3 | Rx | C | N | X |
| Lomaira | 8.1 | Rx | X | 4 | X |
| benzphetamine | 7.6 | Rx | X | 3 | X |
| chorionic gonadotropin (hcg) Off-label | 6.6 | Rx | X | N | |
| desvenlafaxine Off-label | 8.1 | Rx | C | N | X |
| Bontril PDM | 6.0 | Rx | C | 3 | X |
| methamphetamine | 9.2 | Rx | C | 2 | X |
| amphetamine | 10 | Rx | C | 2 | X |
| Imcivree | 9.0 | Rx | N | ||
| methylphenidate Off-label | 6.0 | Rx | C | 2 | X |
| Pregnyl Off-label | 9.0 | Rx | X | N | |
| setmelanotide | 9.0 | Rx | N | ||
| Atti-Plex P | Rx | X | 4 | X | |
| cimetidine Off-label | Rx/OTC | B | N | X | |
| dulaglutide Off-label | Rx | C | N | X | |
| Evekeo | Rx | C | 2 | X | |
| fenfluramine | Rx | C | 4 | X |
|
Legend |
|
| Rating | For ratings, users were asked how effective they found the medicine while considering positive/adverse effects and ease of use (1 = not effective, 10 = most effective). |
| Off-label | This medication may not be approved by the FDA for the treatment of this condition. |
| Rx | Prescription only. |
| OTC | Over-the-counter. |
| Rx/OTC | Prescription or Over-the-counter. |
| Pregnancy Category | Controlled Substances Act (CSA) Schedule | Alcohol | |||
| B | Animal reproduction studies have failed to demonstrate a risk to the fetus and there are no adequate and well-controlled studies in pregnant women. | U | CSA Schedule is unknown. | X | Interacts with Alcohol.
|
| C | Animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use in pregnant women despite potential risks. | N | Is not subject to the Controlled Substances Act. | ||
Management
Reaching and maintaining weight loss for the long term is challenging. It is important that you continue your treatment plan and adopt heart-healthy lifestyle changes you can keep up for the rest of your life. This will help prevent obesity-related complications.
Tips for managing overweight and obesity
Changing lifestyle habits takes time and patience. Follow these tips to help maintain the healthy lifestyle changes your healthcare provider recommended to aim for a healthy weight.
- Use an app on your phone or a journal to record your daily food intake and physical activity. Talk about your goals and your progress with your provider.
- Weigh yourself every day. Daily weighing has been shown to help with initial weight loss as well as long-term weight loss for many people. Purchase a scale to weigh yourself here at iHealth Labs Inc
- Set specific goals. An example of a specific goal is to “walk 30 minutes, 5 days a week” or “eat a serving of vegetables with each meal.” Be realistic about your time and abilities.
- Set doable goals that don’t change too much at once. When starting a new lifestyle, try to avoid changing too much at once. Slow changes lead to success. Remember, quick weight loss methods do not provide lasting results.
- Learn from your slips. Don’t worry if work, the weather, or your family causes you to have an occasional slip. Remember that changing your lifestyle is a long-term process. Find out what triggered the slip and restart your eating and physical activity plan.
- Celebrate your success. Reward yourself along the way as you meet your goals. Instead of eating out to celebrate your success, try a night at the movies, shopping for workout clothes, a visit to the library or bookstore, or a hike.
- Identify temptations. Learn what environments or social activities, such as watching TV or going out with friends, may be keeping you from meeting your goals. Once you have identified the issues, use creative strategies to help keep you on track.
- Plan regular physical activity with a friend. Find a fun activity that you both enjoy, such as Zumba, jogging, biking, or swimming. You are more likely to stick with that activity if you and a friend have committed to it together.
How does obesity affect your health?
Overweight and obesity can directly cause a variety of health problems and indirectly make other health issues more likely to occur. The good news is that losing 5% to 10% of your body weight has meaningful health benefits.
Obesity may cause the following complications:
- Metabolic syndrome
- Type 2 diabetes
- Heart and blood vessel diseases, such as high blood pressure, heart attack, and stroke
- High cholesterol
- Respiratory problems, including asthma, sleep apnea, and obesity hypoventilation syndrome
- Higher risk of serious illness from SARS-CoV-2, the virus that causes COVID-19
- Back pain
- Non-alcoholic fatty liver disease (NAFLD)
- Osteoarthritis, especially in weight-bearing joints such as the knees, because extra weight can damage the cartilage and bone
- Urinary incontinence, which happens when pelvic muscles that are weakened from chronic (long-term) obesity can no longer help maintain bladder control
- Gallbladder disease
- Depression or other mental health conditions
- Cancers, such as pancreatic, colon, breast, and liver cancers
Take care of your mental health
Overweight and obesity can lead to depression or self-esteem issues for people of all ages but especially in children and teens. Obesity and overweight may also lead to or be a sign of an eating disorder.
Talk to your or your child’s provider or a professional counselor. Sometimes a history of childhood trauma, such as emotional neglect, divorce, or substance abuse, is contributing to overweight and obesity. It is important to get professional help for these issues to help you or your child reach and maintain a healthy weight. If you are depressed, your provider may recommend medicines or other treatments that can help.
Support from family and friends can also help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
Childhood Obesity
Childhood obesity is an increasingly serious problem in the United States. Nearly 1 in 5 children have obesity. Children with obesity are more likely to develop other serious health problems, including heart disease and type 2 diabetes. They are also more likely to suffer from anxiety, depression, and low self-esteem.
Obesity affects children from different backgrounds differently. About 1 in 4 Hispanic and non-Hispanic Black children have obesity. This is a challenge for parents, because addressing their child’s weight often means making lifestyle changes for the whole family.
Prevention
All children should visit a healthcare provider every year for wellness check-ups that include monitoring of weight and calculation of body mass index (BMI) percentiles.
Some of the best ways to prevent childhood obesity are to:
- Choose and prepare healthy foods that are lower in fat and have less calories.
- Get regular physical activity. Your children should get at least 60 minutes of daily physical activity.
- Reduce screen time. Try to limit screen time at home to 2 hours or less each day.
- Get enough good-quality sleep.
Risk Factors
Researchers agree that children inherit genes, the blueprints for our bodies, that make them more likely to have obesity. However, that genetic risk does not account for the increase in childhood obesity seen in recent years. A child’s community also has an impact on their weight, as the community can affect a family’s ability to make healthy choices. For example, fresh fruits and vegetables may be difficult to get, roads without sidewalks may make it unsafe to walk for exercise, or healthy meal choices in schools may be unavailable.
Most parents, however, do have some control over other risk factors that increase a child’s risk of having obesity.
These include:
- Eating a high-calorie, low-nutrient diet
- Not getting enough good-quality sleep
- Too much screen time
- Too little physical activity
- Personal or family stress or trauma
BMI for children
BMI is used to determine whether your child’s weight fits the criteria for overweight or obesity. It is compared with growth charts for children who are the same age and sex as your child.
- Underweight is a BMI below the 5th percentile.
- Healthy weight is a BMI between the 5th to the 85th percentile.
- Overweight is a BMI between the 85th percentile and the 95th percentile.
- Obesity is a BMI in the 95th percentile or above.
Treatment
Your child’s provider will monitor your child’s BMI and overall health during regular visits. They may talk to you about healthy lifestyle changes you can make as a family. If your child’s weight does not respond to those, your child’s provider may recommend medicine.
The good news for parents is that childhood obesity is reversible. Even small decreases in weight can have a positive impact on current health and future risk of health problems. The key is to learn the basics of maintaining a healthy weight, seek out resources in your community, and get both medical and mental health care for your child as needed.
Obesity and Women's Health
Women are slightly more likely (40%) than men (35%) to have obesity. Obesity specifically affects some different aspects of women’s health.
- Fertility: Women who have obesity are more likely to have problems getting pregnant than are women who are at a healthy weight.
- Lifetime hormonal changes: Obesity changes reproductive hormone levels as women age.
- Polycystic ovary syndrome (PCOS): PCOS is the most common hormone disorder among women of childbearing age (between about age 15 and 45). Most women with PCOS also have obesity.
- Disease risk: Women with obesity are more likely to have heart disease, diabetes, and breast cancer than are women without obesity.
Pregnancy risks and complications
Having obesity can affect your health and increase the risk of complications during pregnancy and childbirth. Having obesity before pregnancy or gaining too much weight during pregnancy can raise the risk of preterm birth and a baby that is larger than gestational age (larger than they should be at that week of pregnancy). This can lead to problems during delivery for the mother and baby. It can also affect the future health of your child. Talk to your provider about how much weight you should plan to gain during your pregnancy. They can help you set a goal based on your pre-pregnancy BMI.
Several health problems are more common in pregnant women who have obesity. They can cause serious complications during pregnancy.
- Gestational diabetes is typically diagnosed after 20 weeks of pregnancy or close to delivery. It makes it hard for your body to properly break down and store energy from food, causing high levels of glucose in your blood. This can affect both you and your developing baby.
- Gestational hypertension is high blood pressure that starts during the second half of pregnancy.
- Preeclampsia is a combination of high blood pressure during pregnancy with signs that your organs are not working well, such as high protein levels in your urine. It can lead to life-threatening seizures.
- Obstructive sleep apnea happens when your throat muscles relax and you temporarily stop breathing while sleeping. This disrupts your brain’s healthy sleep rhythms and can leave you exhausted upon waking. It can be fatal if severe and not treated.
Your provider will monitor you closely during pregnancy. You should also watch for warning signs of problems, such as high blood pressure, during and after pregnancy. Some warning signs are a worsening headache, overwhelming tiredness, dizziness, trouble breathing, chest or belly pain, swelling, or nausea. If you feel like something is wrong, get medical care right away.
Obesity Hypoventilation Syndrome
What is obesity hypoventilation syndrome?
Obesity hypoventilation syndrome, also known as Pickwickian syndrome, is a breathing disorder that affects some people who have been diagnosed with obesity. Normally, you exhale carbon dioxide, a by-product of breaking down food for energy. Obesity hypoventilation syndrome causes you to have too much carbon dioxide and too little oxygen in your blood. Without treatment, it can lead to serious and even life-threatening health problems.
How do you get it?
Having overweight or obesity increases your risk of developing obesity hypoventilation syndrome. Most people who have obesity hypoventilation syndrome also have sleep apnea.
It is not clear why obesity hypoventilation syndrome affects some people who have obesity and not others. Extra fat on your neck, chest, or across your abdomen can make it difficult to breathe deeply and may produce hormone that affect your body’s breathing patterns. You may also have a problem with the way your brain controls your breathing.
What are the symptoms?
Common symptoms include:
- Breathlessness
- Daytime sluggishness or sleepiness, especially if you also have sleep apnea
- Dizziness
- Fatigue, or extreme tiredness
- Headaches
In addition to the above symptoms, you or a loved one may notice you often snore loudly, choke or gasp, or have trouble breathing at night. Your symptoms may get worse over time.
How is it diagnosed?
If your healthcare provider suspects that you have obesity hypoventilation syndrome, they will:
- Perform a physical exam
- Measure your weight and height
- Calculate your body mass index (BMI)
- Measure your waist and neck circumference
Additional tests might include lung tests to measure the amount of oxygen in your body or how well your lungs are working. You may also need a sleep study if your provider thinks you may have sleep apnea.
How is it treated?
If you are diagnosed with obesity hypoventilation syndrome, your provider may recommend healthy lifestyle changes, such as getting to and maintaining a healthy weight and being physically active. You may also need a continuous positive airway pressure (CPAP) machine or other breathing device at night to help keep your airways open and increase blood oxygen levels. Other treatments may include weight-loss surgery or medicines.
If you have been prescribed a CPAP machine, use it as instructed and continue with your provider’s recommended healthy lifestyle changes to prevent complications. Tell your provider about new symptoms, such as swelling around your ankles, chest pain, lightheadedness, or wheezing. Talk to your provider if you will be flying or need surgery, because these situations can increase your risk for serious complications.
Lifestyle Modifications and Behavior Change
For long-term weight control, lifestyle modifications and behavior change are key. Diet and exercise are important, but so are the psychological and behavioral factors behind obesity. By spotting triggers, finding coping strategies, and practicing mindful eating, lasting changes can be made for a healthier weight.
Identifying Triggers and Developing Coping Strategies
Many people eat emotionally, using food for comfort when stressed, bored, or sad. The first step is to recognize these triggers. Common emotional eating triggers include:
| Trigger | Example | Coping Strategy |
| Stress | Work deadlines, relationship conflicts | Deep breathing, meditation, talking with a friend |
| Boredom | Mindless snacking while watching TV | Engaging in a hobby, going for a walk |
| Sadness | Eating to cope with feelings of loneliness or depression | Journaling, seeking support from loved ones or a therapist |
Creating healthy coping strategies can help manage weight and well-being. This might mean finding new ways to handle stress, like exercise or relaxation, or getting help from a mental health expert.
Mindful Eating and Portion Control Techniques
Mindful eating means focusing on the eating experience without judgment. It helps tune into hunger and fullness signals. This can prevent overeating and lead to better food choices.
Portion control is also vital for weight management. Using smaller plates, measuring food, and being aware of calorie-rich foods helps keep a balanced diet. Small, lasting changes in eating habits can lead to a healthy weight over time.
Support Systems and Resources for Individuals with Obesity
Getting help is key for those fighting obesity. Many support systems and resources are out there. They help people reach their weight loss goals and better their health. These include weight-loss programs, support groups, and professional support from doctors and nutrition experts.
Many weight-loss programs have plans, nutrition advice, and exercise plans made just for you. Some well-known ones are:
| Program | Features |
| Weight Watchers | Point-based system, group meetings, online support |
| Jenny Craig | Prepackaged meals, one-on-one counseling |
| Nutrisystem | Portion-controlled meals, online tools and support |
Joining a support group, online or local, can give you a community feeling. It helps you stay on track. You can share your journey, challenges, and wins with others. There are many obesity resources online, like forums, blogs, and social media groups for weight loss and healthy living.
It’s also important to get help from healthcare providers. Doctors can check your health, find any health issues, and send you to specialists if needed. Dietitians or nutritionists can make meal plans and help with healthy eating. Mental health experts can help with emotional and psychological issues linked to obesity.
By using these support systems and obesity resources, you can get the help and tools you need. This can help you manage your weight and improve your health and happiness.
Call to Action
Obesity is a complex health issue that needs a full approach to prevent and manage. Understanding its causes, risk factors, and effects helps us find ways to manage weight and live healthy lives. A mix of good nutrition, regular exercise, changing habits, and medical help when needed can help keep a healthy weight.
It’s key to see obesity prevention and management as a lifelong journey. It takes commitment, support, and the right resources. By making small, lasting changes and getting help from health experts, we can control our weight and health. Remember, even small steps towards a healthier lifestyle can make a big difference over time.
We must work together to make environments that support healthy choices and weight management. This means pushing for policies that make healthy food more accessible, creating chances for exercise, and reducing obesity stigma. By being proactive and caring, we can fight obesity and improve health for everyone.
So, let’s take action today. If you’re dealing with obesity or want to stay healthy, you’re not alone. Get support from family, doctors, and community groups. Choose healthy foods, stay active, and find positive ways to cope. Together, we can fight the obesity epidemic and create a healthier future for all.
Resources
- Healthfinder.gov Get tips on how to eat healthy on a budget, plan ahead to save time, and eat healthy away from home.
- Nutrition Education Explore materials about menu labeling and the Nutrition Facts label.
- Start Simple with MyPlate App Meet healthy eating goals one at a time! Use this easy-to-use app to get started.
- Foodsafety.gov Learn more about how to keep food safe to eat.
- Purchase a scale to weigh yourself here at iHealth Labs Inc
FAQ's
Q: What is obesity, and how is it defined?
A: Obesity is a condition where you have too much body fat. It can harm your health. Doctors use the Body Mass Index (BMI) to check for obesity. A BMI of 30 or higher means you are obese.
Q: What are the main causes of obesity?
A: Obesity comes from many things. Genetics, lifestyle, and environment play big roles. Poor diet and not moving enough are common causes. Some medical conditions and medicines can also make you gain weight.
Q: What are the health risks associated with obesity?
A: Being obese can lead to serious health issues. These include type 2 diabetes, heart disease, and some cancers. It can also cause joint problems, sleep apnea, and mental health issues. Obesity can make life harder and increase healthcare costs.
Q: How can I determine if I am obese?
A: To check if you’re obese, use the Body Mass Index (BMI). A BMI of 30 or higher means you’re obese. But BMI doesn’t consider muscle or fat distribution. Your doctor might use other methods like waist measurement or body fat percentage.
Q: What role does nutrition play in managing obesity?
A: Nutrition is key in managing obesity. Eating well, controlling portions, and planning meals are important. Choosing healthy foods helps. Getting advice from a dietitian can be very helpful.
Q: How important is physical activity in managing obesity?
A: Exercise is vital for managing obesity. Doing aerobic exercises and strength training helps burn calories and build muscle. Aim for 150 minutes of aerobic activity and muscle-strengthening exercises twice a week.
Q: Are there any medications or surgical options for treating obesity?
A: Yes, there are treatments for obesity. Medications and surgery are options. But, these should be discussed with a doctor. They depend on your health and situation.
Q: What lifestyle changes can I make to manage obesity?
A: Changing your lifestyle is the first step. Eat well, move more, and eat mindfully. Use portion control and find healthy ways to deal with emotions. Small changes can make a big difference over time.
Q: Where can I find support and resources for managing obesity?
A: There are many places to get help for obesity. Look for weight-loss programs, support groups, and professional help. Community centers, hospitals, and online platforms offer resources and support for managing obesity.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 K. Kerr Most recent revision June 28, 2025 08:07:07 AM
**DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE: The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website. |